Здоровый кишечник. Как обрести контроль над весом, настроением и самочувствием [заметки]
1
Yatsunenko, T., et al. “Human Gut Microbiome Viewed across Age and Geography”. Nature 486.7402 (2012): 222–227. Print.
2
Consumer Expenditures in 2009. U. S. Department of Labor. U. S. Bureau of Labor Statistics. May 2011. Report 1028.
3
Исследования, в которых ни участники, ни ученые до конца эксперимента не знают, какая группа принимает плацебо, а какая – реальный препарат. Прим. науч. ред.
4
Robertson, K. L., et al. “Adaptation of the Black Yeast Wangiella Dermatitidis to Ionizing Radiation: Molecular and Cellular Mechanisms”. PLoS One 7.11 (2012): e48674. Print.
5
Schnorr, S. L., et al. “Gut Microbiome of the Hadza Hunter-Gatherers”. Nat Commun 5 (2014): 3654. Print.
6
Yatsunenko, T., et al. “Human Gut Microbiome Viewed across Age and Geography”. Nature 486.7402 (2012): 222–227. Print.
7
De Filippo, C., et al. “Impact of Diet in Shaping Gut Microbiota Revealed by a Comparative Study in Children from Europe and Rural Africa”. Proc Natl Acad Sci U S A 107.33 (2010): 14691–14696. Print. Lin, A., et al. “Distinct Distal Gut Microbiome Diversity and Composition in Healthy Children from Bangladesh and the United States”. PLoS One 8.1 (2013): e53838. Print.
8
Husnik, F., et al. “Horizontal Gene Transfer from Diverse Bacteria to an Insect Genome Enables a Tripartite Nested Mealybug Symbiosis”. Cell 153.7 (2013): 1567–1578. Print.
9
Thompson, J. D. “The Great Stench or the Fool’s Argument”. Yale J Biol Med 64.5 (1991): 529–541. Print.
10
Kendall, A. I. “The Bacteria of the Intestinal Tract of Man”. Science 42.1076 (1915): 209–212. Print.
11
Salyers, A. A., et al. “Fermentation of Mucin and Plant Polysaccharides by Strains of Bacteroides from the Human Colon”. Appl Environ Microbiol 33.2 (1977): 319–322. Print.
12
Финальная стадия процесса расшифровки генома, определение нуклеотидного ряда молекулы ДНК. Прим. ред.
13
Eckburg, P. B., et al. “Diversity of the Human Intestinal Microbial Flora”. Science 308.5728 (2005): 1635–1638. Print.
14
Backhed, F., et al. “The Gut Microbiota as an Environmental Factor That Regulates Fat Storage”. Proc Natl Acad Sci U S A 101.44 (2004): 15718–15723. Print.
15
Ley, R. E., et al. “Obesity Alters Gut Microbial Ecology”. Proc Natl Acad Sci U S A 102.31 (2005): 11070–11075. Print.
16
Turnbaugh, P. J., et al. “An Obesity-Associated Gut Microbiome with Increased Capacity for Energy Harvest”. Nature 444.7122 (2006): 1027–1031. Print.
17
Petersson, J., et al. “Importance and Regulation of the Colonic Mucus Barrier in a Mouse Model of Colitis”. Am J Physiol Gastrointest Liver Physiol 300.2 (2011): G327–G333. Print.
18
Dominguez-Bello, M. G., et al. “Delivery Mode Shapes the Acquisition and Structure of the Initial Microbiota across Multiple Body Habitats in Newborns”. Proc Natl Acad Sci U S A 107.26 (2010): 11971–11975. Print.
19
Lin, P. W., and B. J. Stoll. “Necrotising Enterocolitis”. Lancet 368.9543 (2006): 1271–1283. Print.
20
Claud, E. C., et al. “Bacterial Community Structure and Functional Contributions to Emergence of Health or Necrotizing Enterocolitis in Preterm Infants”. Microbiome 1.1 (2013): 20. Print.
21
Wang, Y., et al. “16S rRNA Gene-Based Analysis of Fecal Microbiota from Preterm Infants with and without Necrotizing Enterocolitis”. ISME J 3.8 (2009): 944–954. Print.
22
Alfaleh, K., and D. Bassler. “Probiotics for Prevention of Necrotizing Enterocolitis in Preterm Infants”. Cochrane Database Syst Rev. 1 (2008): Cd005496. Print.
23
Tarnow-Mordi, W., and R. F. Soll. “Probiotic Supplementation in Preterm Infants: It Is Time to Change Practice”. J Pediatr 164.5 (2014): 959–960. Print.
24
Название штамма бактерий и препарата БАД. Прим. науч. ред.
25
Koren, O., et al. “Host Remodeling of the Gut Microbiome and Metabolic Changes During Pregnancy”. Cell 150.3 (2012): 470–480. Print.
26
Palmer, C., et al. “Development of the Human Infant Intestinal Microbiota”. PLoS Biol 5.7 (2007): e177. Print.
27
De Filippo, C., et al. “Impact of Diet in Shaping Gut Microbiota Revealed by a Comparative Study in Children from Europe and Rural Africa”. Proc Natl Acad Sci U S A 107.33 (2010): 14691–14696. Print.
28
Marcobal, A., “Bacteroides in the Infant Gut Consume Milk Oligosaccharides via Mucus-Utilization Pathways”. Cell Host Microbe 10.5 (2011): 507–514. Print.
29
Cabrera-Rubio, R., et al. “The Human Milk Microbiome Changes over Lactation and Is Shaped by Maternal Weight and Mode of Delivery”. Am J Clin Nutr 96.3 (2012): 544–551. Print.
30
de Weerth, C., et al. “Intestinal Microbiota of Infants with Colic: Development and Specific Signatures”. Pediatrics 131.2 (2013): e550–е558. Print.
31
Koenig, J. E., et al. “Succession of Microbial Consortia in the Developing Infant Gut Microbiome”. Proc Natl Acad Sci U S A 108 Suppl 1 (2011): 4578–4585. Print.
32
Trasande, L., et al. “Infant Antibiotic Exposures and Early-Life Body Mass”. Int J Obes (Lond) 37.1 (2013): 16–23. Print. Hoskin-Parr, L., et al. “Antibiotic Exposure in the First Two Years of Life and Development of Asthma and Other Allergic Diseases by 7.5 Yr: A Dose-Dependent Relationship”. Pediatr Allergy Immunol 24.8 (2013): 762–771. Print.
33
Cho, I., et al. “Antibiotics in Early Life Alter the Murine Colonic Microbiome and Adiposity”. Nature 488.7413 (2012): 621–626. Print.
34
Trasande, L., et al. “Infant Antibiotic Exposures and Early-Life Body Mass”. Int J Obes (Lond) 37.1 (2013): 16–23. Print.
35
Lee, Y. K., et al. “Proinflammatory T-Cell Responses to Gut Microbiota Promote Experimental Autoimmune Encephalomyelitis”. Proc Natl Acad Sci U S A 108 Suppl 1 (2011): 4615–4622. Print.
36
Strachan, D. P. “Hay Fever, Hygiene, and Household Size”. Bmj 299.6710 (1989): 1259–1260. Print.
37
Wlasiuk, G., and D. Vercelli. “The Farm Effect, or, When, What and How a Farming Environment Protects from Asthma and Allergic Disease”. Curr Opin Allergy Clin Immunol 12.5 (2012): 461–466. Print.
38
Savage, J. H., et al. “Urinary Levels of Triclosan and Parabens Are Associated with Aeroallergen and Food Sensitization”. J Allergy Clin Immunol 130.2 (2012): 453–460. e7. Print.
39
Frieden, Thomas. “Antibiotic Resistance and the Threat to Public Health”. Energy and Commerce Subcommittee on Health 2010 of United States House of Representatives. Print.
40
Kozyrskyj, A. L., P. Ernst, and A. B. Becker. “Increased Risk of Childhood Asthma from Antibiotic Use in Early Life”. Chest 131.6 (2007): 1753–1759. Print.
41
Herbst, T., et al. “Dysregulation of Allergic Airway Inflammation in the Absence of Microbial Colonization”. Am J Respir Crit Care Med 184.2 (2011): 198–205. Print.
42
Olszak, T., et al. “Microbial Exposure During Early Life Has Persistent Effects on Natural Killer T Cell Function”. Science 336.6080 (2012): 489–493. Print.
43
Atarashi, K., et al. “Treg Induction by a Rationally Selected Mixture of Clostridia Strains from the Human Microbiota”. Nature 500.7461 (2013): 232–236. Print.
44
Smith, P. M., et al. “The Microbial Metabolites, Short-Chain Fatty Acids, Regulate Colonic Treg Homeostasis”. Science 341.6145 (2013): 569–573. Print.
45
Atherton, J. C., and M. J. Blaser. “Coadaptation of Helicobacter Pylori and Humans: Ancient History, Modern Implications”. J Clin Invest 119.9 (2009): 2475–2487. Print.
46
Song, S. J., et al. “Cohabiting Family Members Share Microbiota with One Another and with Their Dogs”. Elife 2 (2013): e00458. Print.
47
McGovern, P. E., et al. “Fermented Beverages of Pre- and Proto-Historic China”. Proc Natl Acad Sci U S A 101.51 (2004): 17593–17598. Print.
48
Мечников, И. И. Этюды оптимизма. М.: Главная редакция литературы на иностранных языках издательства «Наука», 1988.
49
Merenstein, D., et al. “Use of a Fermented Dairy Probiotic Drink Containing Lactobacillus Casei (DN-114 001) to Decrease the Rate of Illness in Kids: The Drink Study. A Patient-Oriented, Double-Blind, Cluster-Randomized, Placebo-Controlled, Clinical Trial”. Eur J Clin Nutr 64.7 (2010): 669–677. Print.
50
Allen, S. J., et al. “Probiotics for Treating Acute Infectious Diarrhoea”. Cochrane Database Syst Rev. 11 (2010): Cd003048. Print.
51
Hao, Q., et al. “Probiotics for Preventing Acute Upper Respiratory Tract Infections”. Cochrane Database Syst Rev. 9 (2011): Cd006895. Print.
52
Международная научная ассоциация пробиотиков и пребиотиков.
53
В последние годы международное сообщество пытается пересмотреть определение, данное ВОЗ и приведенное в книге, но пока пользуются именно им. И действительно, не все пробиотики проверены в клинических исследованиях. Прим. науч. ред.
54
FDA требует проведения исследований, только если пробиотик планируется использовать для лечения (как лекарство).
55
Sanders, M. E., and J. T. Heimbach. “Functional Foods in the USA: Emphasis on Probiotic Foods”. Food Sci Technol Bull 1.8 (2004): 1–10. Print.
56
Cao, Y., J. Shen, and Z. H. Ran. “Association between Faecalibacterium Prausnitzii Reduction and Inflammatory Bowel Disease: A Meta-Analysis and Systematic Review of the Literature”. Gastroenterol Res Pract2014 (2014): 872725. Print. Fujimoto, T., et al. “Decreased Abundance of Faecalibacterium prausnitzii in the Gut Microbiota of Crohn’s Disease”. J Gastroenterol Hepatol 28.4 (2013): 613–619. Print. Machiels, K., et al. “A Decrease of the Butyrate-Producing Species Roseburia Hominis and Faecalibacterium Prausnitzii Defines Dysbiosis in Patients with Ulcerative Colitis”. Gut 63.8 (2014): 1275–1283. Print. Balamurugan, R., et al. “Real-Time Polymerase Chain Reaction Quantification of Specific Butyrate-Producing Bacteria, Desulfovibrio and Enterococcus Faecalis in the Feces of Patients with Colorectal Cancer”. J Gastroenterol Hepatol 23.8 Pt 1 (2008): 1298–1303. Print.
57
Sokol, H., et al. “Faecalibacterium Prausnitzii Is an Anti-Inflammatory Commensal Bacterium Identified by Gut Microbiota Analysis of Crohn Disease Patients”. Proc Natl Acad Sci U S A 105.43 (2008): 16731–16736. Print.
58
Reid, R. M. “Cultural and Medical Perspectives on Geophagia”. Med Anthropol 13.4 (1992): 337–351. Print.
59
Bittner, A. C., R. M. Croffut, and M. C. Stranahan. “Prescript-Assist Probiotic-Prebiotic Treatment for Irritable Bowel Syndrome: A Methodologically Oriented, 2-Week, Randomized, Placebo-Controlled, Double-Blind Clinical Study”. Clin Ther 27.6 (2005): 755–761. Print.
60
Sonnenburg, E. D., and J. L. Sonnenburg. “Starving Our Microbial Self: The Deleterious Consequences of a Diet Deficient in Microbiota-Accessible Carbohydrates”. Cell Metab (2014). Print.
61
Russell, W. R., et al. “Colonic Bacterial Metabolites and Human Health”. Curr Opin Microbiol 16.3 (2013): 246–254. Print.
62
Torrey, J. C. “The Regulation of the Intestinal Flora of Dogs through Diet”. J Med Res 39.3 (1919): 415–447. Print.
63
Cleave, T. L. The Saccharine Disease: Conditions Caused by the Taking of Refined Carbohydrates, Such as Sugar and White Flour. Keats Publishing, 1975. Print.
64
Trowell, H. C., and D. P. Burkitt. “The Development of the Concept of Dietary Fibre”. Mol Aspects Med 9.1 (1987): 7–15. Print.
65
Martens, E. C., et al. “The Devil Lies in the Details: How Variations in Polysaccharide Fine-Structure Impact the Physiology and Evolution of Gut Microbes”. J Mol Biol (2014). Print.
66
Raninen, K., et al. “Dietary Fiber Type Reflects Physiological Functionality: Comparison of Grain Fiber, Inulin, and Polydextrose”. Nutr Rev 69.1 (2011): 9–21. Print.
67
Dhingra, D., et al. “Dietary Fibre in Foods: A Review”. J Food Sci Technol 49.3 (2012): 255–266. Print. Westenbrink, S., K. Brunt, and J. W. van der Kamp. “Dietary Fibre: Challenges in Production and Use of Food Composition Data”. Food Chem 140.3 (2013): 562–567. Print.
68
Sonnenburg, J. L., et al. “Glycan Foraging in Vivo by an Intestine-Adapted Bacterial Symbiont”. Science 307.5717 (2005): 1955–1959. Print.
69
Johansson, M. E., et al. “Bacteria Penetrate the Normally Impenetrable Inner Colon Mucus Layer in Both Murine Colitis Models and Patients with Ulcerative Colitis”. Gut 63.2 (2014): 281–291. Print.
70
Hehemann, J. H., et al. “Bacteria of the Human Gut Microbiome Catabolize Red Seaweed Glycans with Carbohydrate-Active Enzyme Updates from Extrinsic Microbes”. Proc Natl Acad Sci U S A 109.48 (2012): 19786–19791. Print.
71
Le Chatelier, E., et al. “Richness of Human Gut Microbiome Correlates with Metabolic Markers”. Nature 500.7464 (2013): 541–546. Print.
72
Cotillard, A., et al. “Dietary Intervention Impact on Gut Microbial Gene Richness”. Nature 500.7464 (2013): 585–588. Print.
73
Ridaura, V. K., et al. “Gut Microbiota from Twins Discordant for Obesity Modulate Metabolism in Mice”. Science 341.6150 (2013): 1241214. Print.
74
Kuoliok, K. E. Food and Emergency Food in the Circumpolar Area. Almquist och Wiksell, 1969. Print.
75
Russell, W. R., et al. “High-Protein, Reduced-Carbohydrate Weight-Loss Diets Promote Metabolite Profiles Likely to Be Detrimental to Colonic Health”. Am J Clin Nutr 93.5 (2011): 1062–1072. Print.
76
Koeth, R. A., et al. “Intestinal Microbiota Metabolism of L-Carnitine, a Nutrient in Red Meat, Promotes Atherosclerosis”. Nat Med 19.5 (2013): 576–585. Print.
77
Neufeld, K. M., et al. “Reduced Anxiety-Like Behavior and Central Neurochemical Change in Germ-Free Mice”. Neurogastroenterol Motil 23.3 (2011): 255–264, e119. Print.
78
Diaz Heijtz, R., et al. “Normal Gut Microbiota Modulates Brain Development and Behavior”. Proc Natl Acad Sci U S A 108.7 (2011): 3047–3052. Print.
79
Gareau, M. G., et al. “Bacterial Infection Causes Stress-Induced Memory Dysfunction in Mice”. Gut 60.3 (2011): 307–317. Print.
80
Bercik, P., et al. “The Intestinal Microbiota Affect Central Levels of Brain-Derived Neurotropic Factor and Behavior in Mice”. Gastroenterology 141.2 (2011): 599–609,09. e1–3. Print.
81
Riordan, S. M., and R. Williams. “Gut Flora and Hepatic Encephalopathy in Patients with Cirrhosis”. N Engl J Med 362.12 (2010): 1140–1142. Print.
82
Johnston, G. W., and H. W. Rodgers. “Treatment of Chronic Portal-Systemic Encephalopathy by Colectomy”. Br J Surg 52 (1965): 424–426. Print.
83
Aronov, P. A., et al. “Colonic Contribution to Uremic Solutes”. J Am Soc Nephrol 22.9 (2011): 1769–1776. Print.
84
Wang, Z., et al. “Gut Flora Metabolism of Phosphatidylcholine Promotes Cardiovascular Disease”. Nature 472.7341 (2011): 57–63. Print.
85
Koeth, R. A., et al. “Intestinal Microbiota Metabolism of L–Carnitine, a Nutrient in Red Meat, Promotes Atherosclerosis”. Nat Med 19.5 (2013): 576–585. Print.
86
O’Mahony, S. M., et al. “Maternal Separation as a Model of Brain-Gut Axis Dysfunction”. Psychopharmacology (Berl) 214.1 (2011): 71–88. Print.
87
O’Mahony, S. M., et al. “Early Life Stress Alters Behavior, Immunity, and Microbiota in Rats: Implications for Irritable Bowel Syndrome and Psychiatric Illnesses”. Biol Psychiatry 65 (2009): 263–267. Print.
88
Bailey, M. T., and C. L. Coe. “Maternal Separation Disrupts the Integrity of the Intestinal Microflora in Infant Rhesus Monkeys”. Dev Psychobiol 35.2 (1999): 146–155. Print.
89
Lyte, M., et al. “Induction of Anxiety-Like Behavior in Mice During the Initial Stages of Infection with the Agent of Murine Colonic Hyperplasia Citrobacter Rodentium”. Physiol Behav 89.3 (2006): 350–357. Print. Goehler, L. E., et al. “Campylobacter Jejuni Infection Increases Anxiety-Like Behavior in the Holeboard: Possible Anatomical Substrates for Viscerosensory Modulation of Exploratory Behavior”. Brain Behav Immun22.3 (2008): 354–366. Print.
90
Rao, A. V., et al. “A Randomized, Double-Blind, Placebo-Controlled Pilot Study of a Probiotic in Emotional Symptoms of Chronic Fatigue Syndrome”. Gut Pathog 1.1 (2009): 6. Print. O’Mahony, L., et al. “Lactobacillus and Bifidobacterium in Irritable Bowel Syndrome: Symptom Responses and Relationship to Cytokine Profiles”. Gastroenterology 128.3 (2005): 541–551. Print.
91
Messaoudi, M., et al. “Assessment of Psychotropic-Like Properties of a Probiotic Formulation (Lactobacillus Helveticus R0052 and Bifidobacterium Longum R0175) in Rats and Human Subjects”. Br J Nutr 105.5 (2011): 755–764. Print.
92
Cao, X., et al. “Characteristics of the Gastrointestinal Microbiome in Children with Autism Spectrum Disorder: A Systematic Review”. Shanghai Arch Psychiatry 25.6 (2013): 342–353. Print.
93
Hsiao, E. Y., et al. “Microbiota Modulate Behavioral and Physiological Abnormalities Associated with Neurodevelopmental Disorders”. Cell 155.7 (2013): 1451–1463. Print.
94
Tillisch, K., et al. “Consumption of Fermented Milk Product with Probiotic Modulates Brain Activity”. Gastroenterology 144.7 (2013): 1394–1401, 401.e1–4. Print.
95
Insel, Thomas. “The Top Ten Research Advances of 2012”. National Institute of Mental Health Director’s Blog 2012. Web.
96
DuPont, Herbert L. “Acute Infectious Diarrhea in Immunocompetent Adults”. New Engl J Med 370.16 (2014): 1532.
97
McDonald, L. C., et al. “Vital Signs: Preventing Clostridium difficile Infections”. MMWR Morb Mortal Wkly Rep 61.9 (2012): 1157–1167. Print.
98
Goudarzi, M., et al. “Clostridium difficile Infection: Epidemiology, Pathogenesis, Risk Factors, and Therapeutic Options”. Scientifica 2014 (2014): 916826. Print.
99
van Nood, E., et al. “Duodenal Infusion of Donor Feces for Recurrent Clostridium Difficile”. N Engl J Med 368.5 (2013): 407–415. Print.
100
Eiseman, B., et al. “Fecal Enema as an Adjunct in the Treatment of Pseudomembranous Enterocolitis”. Surgery 44.5 (1958): 854–859. Print.
101
Zhang, F., et al. “Should We Standardize the 1,700-Year-Old Fecal Microbiota Transplantation?” Am J Gastroenterol 107.11 (2012): 1755; author reply pp. 55–56. Print.
102
Dethlefsen, L., and D. A. Relman. “Incomplete Recovery and Individualized Responses of the Human Distal Gut Microbiota to Repeated Antibiotic Perturbation”. Proc Natl Acad Sci U S A 108 Suppl 1 (2011): 4554–4561. Print.
103
Ng, K. M., et al. “Microbiota-Liberated Host Sugars Facilitate Post-Antibiotic Expansion of Enteric Pathogens”. Nature 502.7469 (2013): 96–99. Print.
104
Kashyap, P. C., et al. “Complex Interactions among Diet, Gastrointestinal Transit, and Gut Microbiota in Humanized Mice”. Gastroenterology 144.5 (2013): 967–977. Print.
105
Smith, M. B., C. Kelly, and E. J. Alm. “Policy: How to Regulate Faecal Transplants”. Nature 506.7488 (2014): 290–291. Print.
106
Vrieze, A., et al. “Transfer of Intestinal Microbiota from Lean Donors Increases Insulin Sensitivity in Individuals with Metabolic Syndrome”. Gastroenterology 143.4 (2012): 913–916. e7. Print.
107
van Nood, E., et al. “Fecal Microbiota Transplantation: Facts and Controversies”. Curr Opin Gastroenterol 30.1 (2014): 34–39. Print.
108
Petrof, E. O., et al. “Stool Substitute Transplant Therapy for the Eradication of Clostridium Difficile Infection: ‘Repoopulating’ the Gut”. Microbiome 1.1 (2013): 3. Print.
109
Игра слов: «repopulate» — «восстановить популяцию» и «poop» — «экскременты».
110
Vrieze, A., et al. “Transfer of Intestinal Microbiota from Lean Donors Increases Insulin Sensitivity in Individuals with Metabolic Syndrome”. Gastroenterology 143.4 (2012): 913–916. e7. Print. Nieuwdorp, M., A. Vrieze, and W. M. de Vos. “Reply to Konstantinov and Peppelenbosch”. Gastroenterology 144.4 (2013): e20–е21. Print.
111
Rabbani, G. H., et al. “Green Banana Reduces Clinical Severity of Childhood Shigellosis: A Double-Blind, Randomized, Controlled Clinical Trial”. Pediatr Infect Dis J 28.5 (2009): 420–425. Print.
112
Faith, J. J., et al. “The Long-Term Stability of the Human Gut Microbiota”. Science 341.6141 (2013): 1237439. Print.
113
Lee, S. M., et al. “Bacterial Colonization Factors Control Specificity and Stability of the Gut Microbiota”. Nature 501.7467 (2013): 426–429. Print.
114
Claesson, M. J., et al. “Gut Microbiota Composition Correlates with Diet and Health in the Elderly”. Nature 488.7410 (2012): 178–184. Print.
115
Mueller, S., et al. “Differences in Fecal Microbiota in Different European Study Populations in Relation to Age, Gender, and Country: A Cross-Sectional Study”. Appl Environ Microbiol 72.2 (2006): 1027–1033. Print.
116
Devkota, S., et al. “Dietary-Fat-Induced Taurocholic Acid Promotes Pathobiont Expansion and Colitis in Il10-/- Mice”. Nature 487.7405 (2012): 104–108. Print.
117
Evans, C. C., et al. “Exercise Prevents Weight Gain and Alters the Gut Microbiota in a Mouse Model of High Fat Diet-Induced Obesity”. PLoS One 9.3 (2014): e92193. Print.
118
Viaud, S., et al. “The Intestinal Microbiota Modulates the Anticancer Immune Effects of Cyclophosphamide”. Science 342.6161 (2013): 971–976. Print.
119
Fontana, R. J. “Acute Liver Failure Including Acetaminophen Overdose”. Med Clin North Am. 92.2 (2008): 761–794. Print.
120
Clayton, T. A., et al. “Pharmacometabonomic Identification of a Significant Host-Microbiome Metabolic Interaction Affecting Human Drug Metabolism”. Proc Natl Acad Sci U S A 106.34 (2009): 14728–14733. Print.
121
Wolf, P. “Creativity and Chronic Disease. Vincent van Gogh (1853–1890)”. West J Med 175.5 (2001): 348. Print.
122
Haiser, H. J., et al. “Predicting and Manipulating Cardiac Drug Inactivation by the Human Gut Bacterium Eggerthella Lenta”. Science 341.6143 (2013): 295–298. Print.
123
Biagi, E., et al. “Through Ageing, and Beyond: Gut Microbiota and Inflammatory Status in Seniors and Centenarians”. PLoS One 5.5 (2010): e10667. Print.
124
Cuervo, A., et al. “Fiber from a Regular Diet Is Directly Associated with Fecal Short-Chain Fatty Acid Concentrations in the Elderly”. Nutr Res 33.10 (2013): 811–816. Print.
125
Turnbaugh, P. J., et al. “An Obesity-Associated Gut Microbiome with Increased Capacity for Energy Harvest”. Nature 444.7122 (2006): 1027–1031. Print.
126
Ip, S., et al. “Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries”. Evid Rep Technol Assess (Full Rep) 153 (2007): 1–186. Print.
127
Wlasiuk, G., and D. Vercelli. “The Farm Effect, or, When, What and How a Farming Environment Protects from Asthma and Allergic Disease”. Curr Opin Allergy Clin Immunol 12.5 (2012): 461–466. Print.
128
Hesselmar, B., et al. “Pacifier Cleaning Practices and Risk of Allergy Development”. Pediatrics 131.6 (2013): e1829–е1837. Print.
129
Cotillard, A., et al. “Dietary Intervention Impact on Gut Microbial Gene Richness”. Nature 500.7464 (2013): 585–588. Print.
130
Магазинные кукурузные лепешки можно сделать более мягкими и легко сгибающимися, предварительно подогрев их на сковороде или завернув в мокрую ткань и разогрев в микроволновой печи.
131
Мы держим корень имбиря в морозилке. Замороженный корень хранится несколько месяцев и легко натирается на терке.
132
Мы держим корень имбиря в морозилке. Замороженный корень хранится несколько месяцев и легко натирается на терке.
«Жареные факты» — третья книга Ивана Шишкина, одного из основателей и идеолога кухни московского ресторана Delicatessen, отмеченного гидом «Мишлен». Перед вами экстракт поварской мудрости и остроумия в 137 ответах на вопросы о том как, что и зачем мы едим. Почему в южных странах апельсины не оранжевые, а зеленые, какие курицы летают самолетами, почему с помощью киви легче всего замариновать мясо, можно ли есть медуз и чем опасна ваниль? Вы также найдете здесь два десятка рецептов — от печенья из подсолнечника до черных шотландских яиц — и несчетное количество ценных советов и идей, способных изменить ваш взгляд на приготовление пищи. «Жареные факты» наследуют от предыдущей книги Шишкина, «Под фартуком», не только аптекарскую точность и тонкий юмор, но и команду: редактором выступил Роман Лошманов, автор блога «Вечерний Лошманов», а иллюстрации сделал совладелец Delicatessen Евгений Самолетов, чьи рисунки на бирдекелях стали визитной карточкой места и удостоились издания отдельной книгой.
Гейл Бусси – писательница, художница, профессиональный повар и ведьма домашнего очага. Она живет в деревянном домике у океана на побережье Африки, изучает цветочную терапию, травничество и каждый день творит природную магию. В этой книге она рассказывает о практиках осознанности и любви к волшебному миру природы, а также к себе как части этого огромного прекрасного мира. Книга расскажет о том, как собирать и выращивать цветы и травы, готовить из них изысканные блюда и напитки, варить волшебные зелья, смешивать эфирные масла, проводить несложные ритуалы и по-новому заботиться о своем доме, об уюте, гармонии и о себе: о красоте и совершенстве души и тела. На русском языке публикуется впервые.
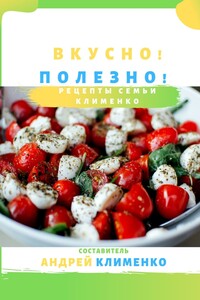
Изысканные салаты, вкуснейшие запеченные блюда из овощей, рыбы и мяса, куриные рулетики, овощное рагу, мидии со сливками и многое другое – от одних только названий уже начинают собираться слюнки и появляется желание пойти в ресторан. Но именно поэтому эта книга для Вас! Правильную, полезную и вкусную еду может приготовить каждый на своей кухне. Данная книга Вам в этом поможет!

В книге рассказывается история главного героя, который сталкивается с различными проблемами и препятствиями на протяжении всего своего путешествия. По пути он встречает множество второстепенных персонажей, которые играют важные роли в истории. Благодаря опыту главного героя книга исследует такие темы, как любовь, потеря, надежда и стойкость. По мере того, как главный герой преодолевает свои трудности, он усваивает ценные уроки жизни и растет как личность.

В книге рассказывается история главного героя, который сталкивается с различными проблемами и препятствиями на протяжении всего своего путешествия. По пути он встречает множество второстепенных персонажей, которые играют важные роли в истории. Благодаря опыту главного героя книга исследует такие темы, как любовь, потеря, надежда и стойкость. По мере того, как главный герой преодолевает свои трудности, он усваивает ценные уроки жизни и растет как личность.

В книге рассказывается история главного героя, который сталкивается с различными проблемами и препятствиями на протяжении всего своего путешествия. По пути он встречает множество второстепенных персонажей, которые играют важные роли в истории. Благодаря опыту главного героя книга исследует такие темы, как любовь, потеря, надежда и стойкость. По мере того, как главный герой преодолевает свои трудности, он усваивает ценные уроки жизни и растет как личность.