Обязательный завтрак, вредный кофе и опасный фастфуд [заметки]
1
Masako N. Dietary walnut supplementation alters mucosal metabolite profiles during DSS-induced colonic ulceration // Nutrients. 2019. Vol. 11. No. 5. P. 1118.
2
Ioannidis J. P. A. The challenge of reforming nutritional epidemiologic research // JAMA. 2018. Vol. 320. No. 10. Pp. 969–970.
3
Ludwig D. S. Improving the quality of dietary research // JAMA. 2019.
5
Лонгитюдное исследование — исследование с многократными фиксациями показателей у одних и тех же участников, позволяющее проверять причинно-следственные гипотезы. Здесь и далее прим. ред., если не указано иное.
6
Однояйцевые (гомозиготные) близнецы — близнецы с идентичным генотипом, которые развились из одной оплодотворенной яйцеклетки. Прим. науч. ред.
7
Nestle M. Unsavory Truth: How Food Companies Skew the Science of What We Eat. Basic Books, 2018.
8
Taylor K. These three companies control everything you buy // Business Insider. 2017. 4 April.
9
Hall K. D. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of food intake // Cell Metabolism. 2019.
10
Spector T. D. Breakfast: a good strategy for weight loss? // BMJ. 2019. 2 February.
11
Astrup A. WHO draft guidelines on dietary saturated and trans fatty acids: time for a new approach? // BMJ. 2019. Vol. 366. P. l4137.
12
Издана на русском языке: Спектор Т. Мифы о диетах. М.: Манн, Иванов и Фербер, 2020.
13
Barabai A. — L. The Unmapped chemical complexity of our diet // Nature Food. 2020. Vol. 1. Pp. 33–37.
16
Велнес (от well — «хорошо», букв. «хорошее самочувствие») — концепция здорового образа жизни, заботы о физическом и ментальном здоровье, правильного питания, отказа от вредных привычек и разумных физических нагрузок.
17
Johnson A. J. Daily sampling reveals personalized diet-microbiome associations in humans // Cell Host & Microbe. 2019. Vol. 25. No. 6. Pp. 789–802.
18
Кейл (кале, кудрявая капуста) — растение семейства капустные, богатое витаминами и минеральными веществами и благодаря этому ставшее популярным в последние годы. Прим. науч. ред.
20
Berry S. E. Decoding human postprandial responses to food and their potential for precision nutrition. PREDICT 1 Study // Nature Medicine. 2020 (in press).
21
Astley C. M. Genetic evidence that carbohydrate-stimulated insulin secretion leads to obesity // Clin. Chem. 2018. Vol. 64. No. 1. Pp. 192–200.
22
Gardner C. D. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: the DIETFITS randomized clinical trial // JAMA. 2018. Feb. 20. Vol. 319. No. 7. Pp. 667–679.
23
Димсам (дим сам) — легкие закуски в китайской кухне, обычно подаваемые с чаем; роти — традиционный индийский хлеб; сааг алу — индийское блюдо из зелени, картофеля и специй. Прим. науч. ред.
24
Sievert K. Effect of breakfast on weight and energy intake: systematic review and meta-analysis of randomised controlled trials // BMJ. 2019. Vol. 364. P. 142.
25
Уровень основного обмена — энергия, которую организм расходует в состоянии покоя. Прим. науч. ред.
26
Betts J. A. Is breakfast the most important meal of the day? // Proceedings of the Nutrition Society. 2016. Vol. 75. No. 4. Pp. 464–474; Casazza K. Weighing the evidence of common beliefs in obesity research // Critical Reviews in Food Science and Nutrition. 2014. Vol. 55. No. 14. Pp. 2014–2053.
27
Jenkins D. J. Nibbling versus gorging: metabolic advantages of increased meal frequency // New England Journal of Medicine. 1989. Vol. 321. No. 14. Pp. 929–934.
28
nhs.uk/live-well/eat-well/eight-tips-for-healthy-eating/ (12 April 2019).
29
Gabel K. Effects of 8-hour time restricted feeding on body weight and metabolic disease risk factors in obese adults: a pilot study // Nutrition and Healthy Aging. 2018. Vol. 4. No. 4. Pp. 345–353; de Cabo R. Effects of intermittent fasting on health, aging and disease // New England Journal of Medicine. 2019. Vol. 381. Pp. 2541–2551.
30
Casazza K. Weighing the evidence of common beliefs in obesity research // Critical Reviews in Food Science and Nutrition. 2014. Vol. 55. No. 14. Pp. 2014–2053.
31
Kaczmarek J. Complex interactions of circadian rhythms, eating behaviors, and the gastrointestinal microbiota and their potential impact on health // Nutrition Reviews. 2017. Vol. 75. No. 9. Pp. 673–682.
32
Adolfus K. The effects of breakfast and breakfast composition on cognition in children and adolescents: a systematic review // Advances in Nutrition. 2016. Vol. 7. No. 3. Pp. 590S–612S.
33
Levine J. Energy expenditure of nonexercise activity // American Journal of Clinical Nutrition. 2000. Vol. 72. No. 6. Pp. 1451–1454.
34
Novotny J. A. Discrepancy between the Atwater factor predicted and empirically measured energy values of almonds in human diet // Am. J. Clin. Nutr. 2012. Vol. 96. No. 2. Pp. 296–301.
35
Carmody R. N. Cooking shapes the structure and function of the gut microbiome // Nature Microbiology. 2019. Vol. 4. No. 12. Pp. 2052–2063.
37
Chaix A. Time-restricted feeding prevents obesity and metabolic syndrome in mice lacking a circadian clock // Cell Metab. 2019. Vol. 29. No. 2. Pp. 303–319.
38
Ebbeling C. Effects of a low carbohydrate diet on energy expenditure during weight loss maintenance: randomized trial // BMJ. 2018. Vol. 363. P. k4583.
39
Gardner C. D. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults // JAMA. 2018. Vol. 319. No. 7. Pp. 667–679.
40
Nunan D. Implausible discussions in saturated fat “research”; definitive solutions won’t come from another million editorials (or a million views of one) // Br. J. Sports Med. 2019. Vol. 53. No. 24. Pp. 1512–1513.
41
nhs.uk/live-well/eat-well/the-eatwell-guide/ (28 January 2019).
42
Zhong V. W. Associations of dietary cholesterol or egg consumption with incident cardiovascular disease and mortality // JAMA. 2019. Vol. 321. No. 11. Pp. 1081–1095.
43
Dehghan M. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study // The Lancet. 2017. Vol. 390. Pp. 2050–2062.
44
Estruch R. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts // New Engl. J. Med. 2018. Vol. 378. No. 25. P. e34.
45
Резолвины — вещества, вырабатываемые организмом из жирных кислот, медиаторы противовоспалительных реакций. В настоящее время их функции активно изучаются. Прим. науч. ред.
46
Serhan C. N. Resolvins in inflammation // J. Clin. Invest. 2018. Vol. 128. No. 7. Pp. 2657–2669.
47
Zhong V. W. Associations of dietary cholesterol or egg consumption with incident cardiovascular disease and mortality // JAMA. 2019. Vol. 321. No. 11. Pp. 1081–1095.
48
Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review // Circulation. 2016. Vol. 133. No. 2. Pp. 187–225.
49
Pimpin L. Is butter back? A systematic review and meta-analysis of butter consumption and risk of cardiovascular disease, diabetes, and total mortality // PLOS ONE. 2016. Vol. 11. No. 6. P. e0158118.
50
Справедливости ради стоит сказать, что пищевая промышленность не синтезирует трансжиры целенаправленно. Это побочный продукт гидрогенизации — превращения ненасыщенных жиров в насыщенные для получения твердых жиров из жидких. Трансжиры в небольших количествах естественным образом присутствуют в натуральных мясных продуктах и в молоке. Прим. науч. ред.
51
Gardner C. D. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults // JAMA. 2018. Vol. 319. No. 7. Pp. 667–679.
52
Hemilä H. Vitamin C for preventing and treating the common cold // Cochrane Database of Systematic Reviews. 2013. Jan. 31. Vol. 1. P. CD000980.
53
Австралазия — термин, использующийся для обозначения региона, включающего в себя Австралию, Новую Гвинею, Новую Зеландию и прилегающие к ним острова Тихого океана.
54
Lippman S. M. Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the Selenium and Vitamin E Cancer Prevention Trial // JAMA. 2009. Vol. 301. No. 1. Pp. 39–51.
55
Vellekkatt F. Efficacy of vitamin D supplementation in major depression: a metaanalysis of randomized controlled trials // Journal of Postgraduate Medicine. 2019. Vol. 65. No. 2. Pp. 74–80; Feldman D. The role of vitamin D in reducing cancer risk and progression // Nature Reviews Cancer. 2014. Vol. 14. No. 5. Pp. 342–357.
56
Trajanoska K. Assessment of the genetic and clinical determinants of fracture risk: genome wide association and mendelian randomisation study // BMJ. 2018. Vol. 362. P. k3225.
57
Ozkan B. Vitamin D intoxication // Turkish Journal of Pediatrics. 2012. Vol. 54. No. 2. Pp. 93–98.
58
В дикорастущих грибах витамин D синтезируется под действием солнечного света, его концентрация невысока и сильно зависит от условий произрастания гриба. Некоторые грибы промышленного производства облучают ультрафиолетом, что стимулирует синтез витамина D. В процессе хранения содержание витамина D в грибах уменьшается. Прим. науч. ред.
59
Bischoff-Ferrari H. A. Monthly high-dose vitamin D treatment for the prevention of functional decline: a randomized clinical trial // JAMA Internal Medicine. 2016. Vol. 176. No. 2. Pp. 175–183; Smith H. Effect of annual intramuscular vitamin D on fracture risk in elderly men and women // Rheumatology. 2007. Vol. 46. No. 12. Pp. 1852–1857.
60
Li K. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort // Heart. 2012. Vol. 98. Pp. 920–925; Anderson J. B. Calcium intake from diet and supplements and the risk of coronary artery calcification and its progression among older adults: 10-year follow-up of the multi-ethnic study of atherosclerosis (MESA) // Journal of the American Heart Association. 2016. Vol. 5. No. 10. P. e003815.
61
Schoenfeld B. J. Is there a postworkout anabolic window of opportunity for nutrient consumption? // Journal of Orthopaedic and Sports Physical Therapy. 2018. Vol. 48. No. 12. Pp. 911–914.
62
Devries M. C. Changes in kidney function do not differ between healthy adults consuming higher-compared with lower- or normal-protein diets: a systematic review and meta-analysis // Journal of Nutrition. 2018. Vol. 148. No. 11. Pp. 1760–1775.
63
Стир-фрай (от англ. stir-fry — «жарить, перемешивая») — популярная в Азии технология приготовления пищи: быстрое обжаривание в раскаленном масле, в глубокой сковороде, при непрерывном перемешивании.
64
Burton-Freeman B. M. Whole food versus supplement: comparing the clinical evidence of tomato intake and lycopene supplementation on cardiovascular risk factors // Advances in Nutrition. 2014. Vol. 5. No. 5. Pp. 457–485.
65
Lippman S. M. Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the Selenium and Vitamin E Cancer Prevention Trial // JAMA. 2009. Vol. 310. No. 1. Pp. 39–51.
66
Abdelhamid A. S. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease // Cochrane Systematic Review. 2018. Vol. 7. P. CD003177.
67
Manson J. E. Marine n-3 fatty acids and prevention of cardiovascular disease and cancer // New England Journal of Medicine. 2019. Vol. 380. No. 1. Pp. 23–32.
68
Khan S. U. Effects of nutritional supplements and dietary interventions on cardiovascular outcomes // Annals of Internal Medicine. 2019. Vol. 171. No. 3. Pp. 190–198.
69
Toews I. Association between intake of non-sugar sweeteners and health outcomes: systematic review and meta-analyses of randomised and non-randomised controlled trials and observational studies // BMJ. 2019. Vol. 364. P. k4718.
70
Dunford E. K. Non-nutritive sweeteners in the packaged food supply — an assessment across 4 countries // Nutrients. 2018. Vol. 10. No. 2. P. e257.
71
Aaron D. G. Sponsorship of national health organizations by two major soda companies // American Journal of Preventative Medicine. 2017. Vol. 52. No. 1. Pp. 20–30.
72
Gornall J. Sugar: spinning a web of influence // BMJ. 2015. Vol. 350. P. h231; infographic doi.org/10.1136/bmj.h231.
73
Veldhuizen M. G. Integration of sweet taste and metabolism determines carbohydrate reward // Current Biology. 2017. Vol. 27. No. 16. Pp. 2476–2485.
74
Blundell J. E. Low-calorie sweeteners: more complicated than sweetness without calories // American Journal of Clinical Nutrition. 2019. Vol. 109. No. 5. Pp. 1237–1238.
75
Suez J. Artificial sweeteners induce glucose intolerance by altering the gut microbiota // Nature. 2014. Vol. 514. No. 7521. Pp. 181–186.
76
Ruiz-Ojeda F. J. Effects of sweeteners on the gut microbiota: a review of experimental studies and clinical trials // Advances in Nutrition. 2019. Vol. 10. Pp. s31–s48.
77
Daly K. Bacterial sensing underlies artificial sweetener-induced growth of gut Lactobacillus // Environmental Microbiology. 2016. Vol. 18. No. 7. Pp. 2159–2171.
78
79
Higgins K. A. A randomized controlled trial contrasting the effects of 4 low-calorie sweeteners and sucrose on body weight in adults with overweight or obesity // American Journal of Clinical Nutrition. 2019. Vol. 109. No. 5. Pp. 1288–1301.
80
Olsson K. Microbial production of next-generation stevia sweeteners // Microbial Cell Factories. 2016. Vol. 15. No. 1. P. 207.
81
82
Wang Q. P. Non-nutritive sweeteners possess a bacteriostatic effect and alter gut microbiota in mice // PLOS ONE. 2018. Vol. 13. No. 7. P. e0199080.
83
Цикута (вёх ядовитый) — токсичное растение семейства зонтичные, широко распространенное на территории Восточной Европы и Северной Америки. Прим. науч. ред.
84
Borges M. C. Artificially sweetened beverages and the response to the global obesity crisis // PLOS Medicine. 2017. Vol. 14. No. 1. P. e1002195.
85
Cowburn G. Consumer understanding and use of nutrition labelling: a systematic review // Public Health Nutrition. 2005. Vol. 8. No. 1. Pp. 21–28.
86
Geiger C. J. Health claims: history, current regulatory status, and consumer research // Journal of the American Dietetic Association. 1998. Vol. 98. No. 11. Pp. 1312–1314.
87
В России норма физиологических потребностей в пищевых волокнах (клетчатке) для взрослых составляет 20 г (согласно МР 2.3.1.2432–08 Нормы физиологических потребностей в энергии и пищевых веществах для различных групп населения Российской Федерации). Прим. науч. ред.
88
DuBroff R. Fat or fiction: the diet-heart hypothesis // BMJ Evidence-Based Medicine. 2019. 29 May. P. ii: bmjebm-2019–111180.
90
Goiana-da-Silva F. Front-of-pack labelling policies and the need for guidance // Lancet Public Health. 2019. Vol. 4. No. 1. P. PE15.
91
Estruch R. Primary prevention of cardiovascular disease with a Mediterranean diet // New England Journal of Medicine. 2013. Vol. 368. Pp. 1279–1290.
92
Ares G. Comparative performance of three interpretative front-of-pack nutrition labelling schemes: insights for policy making // Food Quality and Preference. 2018. Vol. 68. Pp. 215–225.
93
Acton R. B. Do consumers think front-of-package “high in” warnings are harsh or reduce their control? // Obesity. 2018. Vol. 26. No. 11. Pp. 1687–1691.
94
Cecchini M. Impact of food labelling systems on food choices and eating behaviors: a systematic review and meta-analysis of randomized studies // Obes. Rev. Mar. 2016. Vol. 17. No. 3. Pp. 201–210.
95
Bleich S. N. Diet-beverage consumption and caloric intake among US adults, overall and by body weight // American Journal of Public Health. 2014. Vol. 104. Pp. e72–e78.
96
Petimar J. Estimating the effect of calorie menu labeling on calories purchased in a large restaurant franchise in the southern United States: quasi-experimental study // BMJ. 2019. Vol. 367. P. l5837.
97
Downs J. S. Supplementing menu labeling with calorie recommendations to test for facilitation effects // American Journal of Public Health. 2012. Vol. 103. Pp. 1604–1609.
98
Monteiro C. A. NOVA. The star shines bright // World Nutrition. 2016. Vol. 7. No. 1–3. Pp. 28–38.
99
Monteiro C. A. Household availability of ultra-processed foods and obesity in nineteen European countries // Public Health Nutrition. 2018. Vol. 21. No. 1. Pp. 18–26.
100
Steele E. M. Ultra-processed foods and added sugars in the US diet: evidence from a nationally representative cross-sectional study // BMJ Open. 2016. Vol. 6. P. e009892.
101
Hall K. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake // Cell Metabolism. 2019. Vol. S1550–4131. No. 19. Pp. 30248–30257.
102
Poti J. M. Ultra-processed food intake and obesity: what really matters for health — processing or nutrient content? // Current Obesity Reports. 2012. Vol. 6. No. 4. Pp. 420–431.
103
Kong L. C. Dietary patterns differently associate with inflammation and gut microbiota in overweight and obese subjects // PLOS ONE. 2014. Vol. 9. No. 10. P. e109434.
104
Mendonça R. Ultraprocessed food consumption and risk of overweight and obesity // American Journal of Clinical Nutrition. 2016. Vol. 104. No. 5. Pp. 1433–1440; Mozzaffarian D. Changes in diet and lifestyle and long-term weight gain in women and men // New England Journal of Medicine. 2011. Vol. 364. No. 25. Pp. 2392–2404.
105
Bouzari A. Vitamin retention in eight fruits and vegetables: a comparison of refrigerated and frozen storage // Journal of Agricultural and Food Chemistry. 2015. Vol. 63. No. 3. Pp. 957–962.
106
107
Bouvard V. Carcinogenicity of consumption of red and processed meat // The Lancet Oncology. 2015. Vol. 16. No. 16. Pp. 1599–1600.
108
Plant-based meat could create a radically different food chain // The Economist. 12 October 2019.
109
Dehghan M. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study // The Lancet. 2017. Vol. 390. No. 10107. Pp. 2050–2062.
110
Wang X. Red and processed meat consumption and mortality: dose-response metaanalysis of prospective cohort studies // Public Health Nutrition. 2016. Vol. 19. No. 5. Pp. 893–905; Etemadi A. Mortality from different causes associated with meat, heme iron, nitrates, and nitrites in the NIH-AARP Diet and Health Study // BMJ. 2017. Vol. 357. P. j1957.
111
Zeraatkar D. Red and processed meat consumption and risk for all-cause mortality and cardiometabolic outcomes: a systematic review and meta-analysis of cohort studies // Ann. Intern. Med. 2019. Vol. 171. No. 10. Pp. 721–731.
112
Rubin R. Blacklash over meat dietary recommendations raises questions about corporate lies to nutrition scientists // JAMA. 2020.
113
Spector T. D. Bacon rashers, statistics, and controversy // blog.bmj.com. 9 October 2019.
114
Lee J. E. Meat intake and cause-specific mortality: a pooled analysis of Asian prospective cohort studies // American Journal of Clinical Nutrition. 2013. Vol. 98. No. 4. Pp. 1032–1041.
115
Lanza E. The polyp prevention trial continued follow-up study // Cancer Epidemiology, Biomarkers and Prevention. 2007. Vol. 16. No. 9. Pp. 1745–1752; Thomson C. A. Cancer incidence and mortality during the intervention and post intervention periods of the Women’s Health Initiative Dietary Modification Trial // Cancer Epidemiology, Biomarkers and Prevention. 2014. Vol. 23. No. 12. Pp. 2924–2935.
116
Bouvard V. Carcinogenicity of consumption of red and processed meat // The Lancet Oncology. 2015. Vol. 16. No. 16. Pp. 1599–1600.
117
Anderson J. J. Red and processed meat consumption and breast cancer: UK Biobank cohort study and meta-analysis // Eur. J. Cancer. 2018. Vol. 90. Pp. 73–82.
118
Średnicka-Tober D. Composition differences between organic and conventional meat: a systematic literature review and meta-analysis // Br. J. Nutr. 2016. Vol. 115. No. 6. Pp. 994–1011.
119
Willett W. Food in the Anthropocene: the EAT-Lancet commission on healthy diets from sustainable food systems // The Lancet. 2019. Vol. 393. Pp. 447–492.
120
Poore J. Reducing food’s environmental impacts through producers and consumers // Science. 2018. Vol. 360. No. 6392. Pp. 987–992.
121
Springmann M. Options for keeping the food system within environmental limits // Nature. 2018. Vol. 562. Pp. 519–525.
122
Springmann M. Health-motivated taxes on red and processed meat: a modelling study on optimal tax levels and associated health impacts // PLOS ONE. 2018. Vol. 13. No. 11. P. e0204139.
123
Capper J. L. The environmental impact of beef production in the United States: 1977 compared with 2007 // Journal of Animal Science. 2011. Vol. 89. Pp. 4249–4261.
124
Lopez A. Iron deficiency anemia // The Lancet. 2016. Vol. 387. No. 10021. Pp. 907–916.
125
Mentre A. Evolving evidence about diet and health // The Lancet Public Health. 2018. Vol. 3. No. 9. Pp. e408–e409; Jacka F. N. Association of Western and traditional diets with depression and anxiety in women // American Journal of Psychiatry. 2010. Vol. 167. No. 3. Pp. 305–311.
126
Jacka F. N. Red meat consumption and mood and anxiety disorders // Psychotherapy and Psychosomatics. 2012. Vol. 81. No. 3. Pp. 196–198.
127
Daley C. A. A review of fatty acid profiles and antioxidant content in grass-fed and grain-fed beef // Nutrition Journal. 2010. Vol. 9. No. 1. P. 10.
128
Pelucchi C. Dietary acrylamide and cancer risk: an updated meta-analysis // International Journal of Cancer. 2015. Vol. 136. Pp. 2912–2922.
129
Lee J. G. Effects of grilling procedures on levels of polycyclic aromatic hydrocarbons in grilled meats // Food Chemistry. 2016. Vol. 199. Pp. 632–638; Stec A. A. Occupational exposure to polycyclic aromatic hydrocarbons and elevated cancer incidence in firefighters // Scientific Reports. 2018. Vol. 8. No. 1. P. 2476.
130
Скампи (итал. scampi) — крупная морская креветка с длинными тонкими клешнями; другие названия: норвежский омар, дублинская креветка, лангустин. В итальянской кухне таких креветок поджаривают на гриле: шейки маринуют в оливковом масле с чесноком и жарят на шампурах; также иногда их употребляют в сыром виде (scampi crudi).
131
Gifford C. L. Broad and inconsistent muscle food classification is problematic for dietary guidance in the US // Nutrients. 2017. Vol. 9. No. 9. P. 1027.
132
Bergeron N. Effects of red meat, white meat, and nonmeat protein sources on atherogenic lipoprotein measures in the context of low compared with high saturated fat intake: a randomized controlled trial // Am. J. Clin. Nutr. 2019. Jun. 4: online.
133
EFSA. Opinion of the scientific panel on food additives, flavorings, processing aids and materials in contact with food (AFC) related to treatment of poultry carcasses with chlorine dioxide, acidified sodium chlorite, trisodium phosphate and peroxyacids // European Food Safety Authority. 2006. Vol. 4. No. 1. P. 297.
134
Harvey F. British supermarket chickens show record levels of antibioticresistant superbugs // The Guardian. 2018. January 15.
135
Lawrence F. Revealed: the dirty secret of the UK’s poultry industry // The Guardian. 2014. July 23.
136
Преимущественно растительная диета с небольшой долей продуктов животного происхождения в рационе.
137
Raji C. A. Regular fish consumption and age-related brain gray matter loss // American Journal of Preventive Medicine. 2014. Vol. 47. No. 4. Pp. 444–451.
138
Morris M. C. Fish consumption and cognitive decline with age in a large community study // Archives of Neurology. 2005. Vol. 62. No. 12. Pp. 1849–1853.
139
Короткоцепочечными принято считать кислоты с длиной цепи меньше 6 атомов углерода, поэтому альфа-линоленовая кислота не является короткоцепочечной (в ней 18 атомов углерода). В ЭПК 20 атомов углерода, в ДГК 21 атом углерода. Прим. науч. ред.
140
Saunders A. V. Omega-3 polyunsaturated fatty acids and vegetarian diets // Medical Journal of Australia. 2013. Vol. 1. No. 2. Pp. 22–26.
141
Stonehouse W. Does consumption of LC omega-3 PUFA enhance cognitive performance in healthy school-aged children and throughout adulthood? Evidence from clinical trials // Nutrients. 2014. Vol. 6. No. 7. Pp. 2730–2758; Cooper R. E. Omega-3 polyunsaturated fatty acid supplementation and cognition: a systematic review & metaanalysis // Journal of Psychopharmacology. 2015. Vol. 29. No. 7. Pp. 753–763.
142
Øyen J. Fatty fish intake and cognitive function: FINS-KIDS, a randomized controlled trial in preschool children // BMC Medicine. 2018. Vol. 16. P. 41.
143
Gould J. F. Seven-year follow-up of children born to women in a randomized trial of prenatal DHA supplementation // JAMA. 2017. Vol. 317. No. 11. Pp. 1173–1175.
144
Engeset D. Fish consumption and mortality in the European Prospective Investigation into Cancer and Nutrition cohort // European Journal of Epidemiology. 2015. Vol. 30. No. 1. Pp. 57–70.
145
Schwingshackl L. Food groups and risk of all-cause mortality: a systematic review and meta-analysis // American Journal of Clinical Nutrition. 2017. Vol. 105. No. 6. Pp. 1462–1473.
146
Song M. Association of animal and plant protein intake with all-cause and causespecific mortality // JAMA Internal Medicine. 2016. Vol. 176. No. 10. Pp. 1453–1463.
147
Siscovick D. S. Omega-3 polyunsaturated fatty acid (fish oil) supplementation and the prevention of clinical cardiovascular disease: a science advisory from the American Heart Association // Circulation. 2017. Vol. 135. No. 15. Pp. e867–e884.
148
Aung T. Associations of omega-3 fatty acid supplement use with CVD risks: metaanalysis of 10 trials involving 77,917 individuals // JAMA Cardiology. 2018. Vol. 3. No. 3. Pp. 225–234.
149
Abdelhamid A. S. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease // Cochrane Systematic Review. 2018. Vol. 7. P. CD003177.
150
Manson J. E. Marine n–3 fatty acids and prevention of cardiovascular disease and cancer // New England Journal of Medicine. 2019. Vol. 380. Pp. 23–32.
151
Senftleber N. K. Marine oil supplements for arthritis pain: a systematic review and meta-analysis of randomized trials // Nutrients. 2017. Vol. 9. No. 1. P. e42.
152
Астаксантин — природный пигмент, придающий различным видам рыб, морских животных, водорослям и перьям птиц красную окраску. В организме человека выполняет функцию антиоксиданта, способствует поддержанию остроты зрения. Прим. науч. ред.
153
Tacon A. G. Global overview on the use of fish meal and fish oil in industrially compounded aquafeeds // Aquaculture. 2008. Vol. 285. No. 1–4. Pp. 146–158.
154
Poore J. Reducing food’s environmental impacts through producers and consumers // Science. 2018. Vol. 360. No. 6392. Pp. 987–992.
155
Han Y. Fishmeal application induces antibiotic resistance gene propagation in mariculture sediment // Environmental Science and Technology. 2017. Vol. 51. No. 18. Pp. 10850–10860.
156
Whittle P. Plagues of parasitic sea lice depleting world’s salmon stocks // The Independent. 19 September 2017.
157
Khan S. Scottish salmon sold by a range of supermarkets in the UK has sea lice up to 20 times the acceptable amount // The Independent. 29 October 2017.
158
Christensen J. Fish fraud: what’s on the menu often isn’t what’s on your plate // CNN. March 7, 2019.
159
Warner K. Deceptive dishes: seafood swaps found worldwide // Oceana Report. 7 September 2016.
160
Willette D. A. Using DNA barcoding to track seafood mislabeling in Los Angeles restaurants // Conservation Biology. 2017. Vol. 31. No. 5. Pp. 1076–1085.
161
Gander K. Fraudsters are dyeing cheap tuna pink and selling it on as fresh fish in £174m industry // The Independent. 18 January 2017.
162
Kuchta R. Diphyllobothrium nihonkaiense tapeworm larvae in salmon from North America // Emerging Infectious Diseases. 2017. Vol. 23. No. 2. Pp. 351–353.
163
Iwata K. Is the quality of sushi ruined by freezing raw fish and squid? A randomized double-blind trial // Clinical Infectious Diseases. 2015. Vol. 60. No. 9. Pp. e43–e48.
164
Planchart A. Heavy metal exposure and metabolic syndrome: evidence from human and model system studies // Current Environmental Health Reports. 2018. Vol. 5. No. 1. Pp. 110–124.
165
Oken E. Fish consumption, methylmercury and child neurodevelopment // Current Opinion in Pediatrics. 2008. Vol. 20. No. 2. Pp. 178–183; Sagiv S. K. Prenatal exposure to mercury and fish consumption during pregnancy and attention-deficit/hyperactivity disorder-related behavior in children // Archives of Pediatrics and Adolescent Medicine. 2012. Vol. 166. No. 12. Pp. 1123–1131.
166
Galloway T. S. Marine microplastics spell big problems for future generations // Proceedings of the National Academy of Sciences. 2016. Vol. 113. No. 9. Pp. 2331–2333.
167
Abdelhamid A. S. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease // Cochrane Systematic Review. 2018. Vol. 7. P. CD003177.
169
Люди, родившиеся в период примерно с 1981 по 1996 год. Прим. науч. ред.
170
Losasso C. Assessing influence of vegan, vegetarian and omnivore oriented Westernized dietary styles on human gut microbiota // Frontiers in Microbiol. 2018. Vol. 9. P. 317.
171
Benatar J. R. Cardiometabolic risk factors in vegans; A meta-analysis of observational studies // PLOS ONE. 2018. Vol. 13. No. 12. P. e0209086.
172
Kahleova H. Cardio-metabolic benefits of plant-based diets // Nutrients. 2017. Vol. 9. No. 8. P. 848.
173
Orlich M. J. Vegetarian dietary patterns and mortality in Adventist Health Study 2 // JAMA Internal Medicine. 2013. Vol. 173. No. 13. Pp. 1230–1238.
174
Fønnebø V. The healthy Seventh-Day Adventist lifestyle: what is the Norwegian experience? // American Journal of Clinical Nutrition. 1994. Vol. 59. No. 5. Pp. 1124S–1129S.
175
Mihrshahi S. Vegetarian diet and all-cause mortality: evidence from a large population-based Australian cohort — the 45 and Up Study // Preventative Medicine. 2017. Vol. 97. Pp. 1–7.
176
Appleby P. N. Mortality in vegetarians and comparable nonvegetarians in the United Kingdom // American Journal of Clinical Nutrition. 2016. Vol. 103. No. 1. Pp. 218–230.
177
Segovia-Siapco G. Health and sustainability outcomes of vegetarian dietary patterns: a revisit of the EPIC-Oxford and the Adventist Health Study 2 cohorts // Eur. J. Clin. Nutr. Jul. 2019. Vol. 72. No. Suppl. 1. Pp. 60–70.
178
Turner-McGrievy G. M. A two-year randomized weight loss trial comparing a vegan diet to a more moderate low-fat diet // Obesity. 2012. Vol. 15. Pp. 2276–2281.
179
Fothergill E. Persistent metabolic adaptation 6 years after “The Biggest Loser” competition // Obesity. 2016. Vol. 24. Pp. 1612–1619.
180
Barthels F. Orthorexic and restrained eating behaviour in vegans, vegetarians, and individuals on a diet // Eat Weight Disord. 2018. Vol. 23. No. 2. Pp. 159–166.
181
Утверждение автора не соответствует действительности. В США, согласно Dietary Guidelines for Americans, рекомендовано употреблять 14 г клетчатки на 1000 ккал энергетической ценности рациона, то есть от 25 г в день, в Великобритании — 30 г в день. В России взрослым рекомендовано употреблять 20 г пищевых волокон в сутки. Прим. науч. ред.
182
Veronese N. Dietary fiber and health outcomes: an umbrella review of systematic reviews and meta-analyses // Am. J. Clin. Nutr. 2018. Vol. 107. No. 3. Pp. 436–444.
183
Billingsley H. E. The antioxidant potential of the Mediterranean diet in patients at high cardiovascular risk: in-depth review of PREDIMED // Nutrition and Diabetes. 2018. Vol. 8. No. 1. P. 13; Subash S. Neuroprotective effects of berry fruits on neurodegenerative diseases // Neural Regeneration Research. 2014. Vol. 9. No. 16. Pp. 1557–1566.
184
Bolland M. J. Calcium intake and risk of fracture: systematic review // BMJ. 2015. Vol. 351. P. h4580.
185
waterfootprint.org/en/resources/waterstat/ (November 2019).
186
Whitton C. National Diet and Nutrition Survey: UK food consumption and nutrient intakes // British Journal of Nutrition. 2011. Vol. 106. No. 12. Pp. 1899–1914.
187
Clarys P. Dietary pattern analysis: a comparison between matched vegetarian and omnivorous subjects // Nutrition Journal. 2013. Vol. 12. P. 82.
188
Lynch H. Plant-based diets: considerations for environmental impact, protein quality, and exercise performance // Nutrients. 2018. Vol. 10. No. 12. Pp. 1841.
189
Pawlak R. The prevalence of cobalamin deficiency among vegetarians assessed by serum vitamin B12: a review // European Journal of Clinical Nutrition. 2014. Vol. 68. No. 5. Pp. 541–548.
190
Haider L. M. The effect of vegetarian diets on iron status in adults: a systematic review and meta-analysis // Critical Reviews in Food Science & Nutrition. 2018. Vol. 58. No. 8. Pp. 1359–1374.
191
Saunders T. A. Growth and development of British vegan children // American Journal of Clinical Nutrition. 1988. Vol. 48. No. 3. Pp. 822–825; Sunderland M. Judge convicts parents after baby dies from vegan diet // Vice. 15 June 2017.
192
Webb M. Cost effectiveness of a government supported policy strategy to decrease sodium intake: global analysis across 183 nations // BMJ. 2019. Vol. 356. P. i6699.
193
Trieu K. Salt reduction initiatives around the world — a systematic review of progress towards the global target // PLOS ONE. 2015. Vol. 10. No. 7. P. e0130247.
194
Hidden salt present in popular restaurant meals // BBC News online. 11 March 2013.
195
Moran A. J. Consumer underestimation of sodium in fast food restaurant meals // Appetite. 2017. Vol. 113. Pp. 155–161.
196
Luft K. Influence of genetic variance on sodium sensitivity of blood pressure // Klin. Wochenschr. 1987. Vol. 65. No. 3. Pp. 101–109.
197
Dong O. Excessive dietary sodium intake and elevated blood pressure: a review of current prevention and management strategies and the emerging role of pharmaconutrigenetics // BMJ Nutrition Prevention & Health. 2018. Vol. 1 // doi: 10.1136.
198
Graudal N. A. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride // Cochrane Database Syst. Rev. 9 April 2017. Vol. 4. P. CD004022.
199
Adler A. J. Reduced dietary salt for the prevention of cardiovascular disease // Cochrane Database Syst. Rev. 2014. Vol. 12. P. CD009217.
200
Chang H. Y. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men // Am. J. Clin. Nutr. 2006. Vol. 83. No. 6. Pp. 1289–1296.
201
Ekinci E. I. Dietary salt intake and mortality in patients with type 2 diabetes // Diabetes Care. 2011. Vol. 34. No. 3. Pp. 703–709.
202
Townsend R. R. Salt intake and insulin sensitivity in healthy human volunteers // Clinical Science. 2007. Vol. 113. No. 3. Pp. 141–148.
203
Mente A. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality // The Lancet. 2018. Vol. 392. No. 10146. Pp. 496–506.
204
Cappuccio F. P. Population dietary salt reduction and the risk of cardiovascular disease. A scientific statement from the European Salt Action Network // Nutr. Metab. Cardiovasc. Dis. 2018. Vol. 29. No. 2. Pp. 107–114.
205
Лизин — одна из незаменимых аминокислот, в больших количествах содержится в бобовых и в гречневой крупе. Прим. науч. ред.
206
Chiavaroli L. DASH dietary pattern and cardiometabolic outcomes: an umbrella review of systematic reviews and meta-analyses // Nutrients. 2019. Vol. 11. No. 2. P. pii: E338.
207
Scott-Thomas C. Salt replacements could be deadly, say renal specialists // FoodNavigator. 19 March 2009.
208
He K. Consumption of monosodium glutamate in relation to incidence of overweight in Chinese adults: China Health and Nutrition Survey (CHNS) // Am. J. Clin. Nutr. 2011. Vol. 93. No. 6. Pp. 1328–1336.
209
Yang Q. Q. Improved growth performance, food efficiency, and lysine availability in growing rats fed with lysine-biofortified rice // Sci. Rep. 2017. Vol. 7. No. 1. P. 1389.
210
Boston Collaborative Drug Surveillance Program. Coffee drinking and acute myocardial infarction // The Lancet. 1972. Vol. 300. No. 7790. Pp. 1278–1281; Jick H. Coffee and myocardial infarction // New England Journal of Medicine. 1973. Vol. 289. No. 2. Pp. 63–67.
211
Zuchinali P. Effect of caffeine on ventricular arrhythmia: a systematic review and meta-analysis of experimental and clinical studies // EP Europace. 2016. Vol. 18. No. 2. Pp. 257–266.
212
Ding M. Long-term coffee consumption and risk of cardiovascular disease: systematic review and a dose-response meta-analysis // Circulation. 2013. Vol. 129. No. 6. Pp. 643–659.
213
Crippa A. Coffee consumption and mortality from all causes, CVD, and cancer: a dose-response meta-analysis // Am. Journal of Epidemiology. 2014. Vol. 180. No. 8. Pp. 763–775.
214
Parker J. K. Kinetic model for the formation of acrylamide during the finish-frying of commercial French Fries // J. Agricultural and Food Chemistry. 2012. Vol. 60. No. 32. Pp. 9321–9331.
215
Devlin H. How burnt toast and roast potatoes became linked to cancer // The Guardian. 27 January 2017.
216
Marx B. Mécanismes de l’effet diurétique de la caffeine’ // Médecine Sciences. 2016. Vol. 32. No. 5. Pp. 485–490.
217
Liu Q. P. Habitual coffee consumption and risk of cognitive decline/dementia: a systematic review and meta-analysis // Nutrition. 2016. Vol. 32. No. 6. Pp. 628–636; Ross G. W. Association of coffee and caffeine intake with the risk of Parkinson disease // JAMA. 2000. Vol. 283. No. 20. Pp. 2674–2679.
218
Pickering C. Caffeine and exercise: what next? // Sports Medicine. 2019. Vol. 49. No. 7. Pp. 1007–1030.
219
Snel J. Effects of caffeine on sleep and cognition // Progress in Brain Research. 2011. Vol. 190. Pp. 105–117.
220
Winston A. P. Neuropsychiatric effects of caffeine // Advances in Psychiatric Treatment. 2005. Vol. 11. No. 6. Pp. 432–439.
221
Lucas M. Coffee, caffeine, and risk of depression among women // Archives of Internal Medicine. 2011. Vol. 171. No. 17. Pp. 1571–1578.
222
Lucas M. Coffee, caffeine, and risk of completed suicide: results from three prospective cohorts of American adults // World Journal of Biological Psychiatry. 2012. Vol. 15. No. 5. Pp. 377–386.
223
Coelho C. Nature of phenolic compounds in coffee melanoidins // Journal of Agricultural and Food Chemistry. 2014. Vol. 62. No. 31. Pp. 7843–7853.
224
Gniechwitz D. Dietary fiber from coffee beverage: degradation by human fecal microbiota // Journal of Agricultural and Food Chemistry. 2007. Vol. 55. No. 17. Pp. 6989–6996.
225
Flaten M. A. Expectations and placebo responses to caffeine-associated stimuli // Psychopharmacology. 2003. Vol. 169. No. 2. Pp. 198–204; Benke C. Effects of anxiety sensitivity and expectations on the startle eyeblink response during caffeine challenge // Psychopharmacology. 2015. Vol. 232. No. 18. Pp. 3403–3416.
226
Mills L. Placebo caffeine reduces withdrawal in abstinent coffee drinkers // Psychopharmacology. 2016. Vol. 30. No. 4. Pp. 388–394.
227
EFSA. EFSA opinion on the safety of caffeine. 23 June 2015.
228
Teucher B. Dietary patterns and heritability of food choice in a UK female twin cohort // Twin Research and Human Genetics. 2007. Vol. 10. No. 5. Pp. 734–748.
229
Dulloo A. G. Normal caffeine consumption: influence on thermogenesis and daily energy expenditure in lean and postobese human volunteers // American Journal of Clinical Nutrition. 1989. Vol. 49. No. 1. Pp. 44–50.
230
Doherty M. Effects of caffeine ingestion on rating of perceived exertion during and after exercise: a meta-analysis // Medicine and Science in Sports. 2005. Vol. 15. No. 2. Pp. 69–78.
231
nhs.uk/conditions/pregnancy-and-baby/foods-to-avoid-pregnant/ (23 January 2017); acog.org/Patients/FAQs/Nutrition-During-Pregnancy? (February 2018).
232
Rhee J. Maternal caffeine consumption during pregnancy and risk of low birth weight: A Dose-response meta-analysis // PLOS ONE. 2015. Vol. 10. No. 7. P. e0132334.
233
Holst L. Raspberry leaf — should it be recommended to pregnant women? // Complementary Therapies in Clinical Practice. 2009. Vol. 15. No. 4. Pp. 204–208.
234
Kennedy D. A. Safety classification of herbal medicines used in pregnancy in a multinational study // BMC Complementary Alternative Medicine. 2016. Vol. 16. No. 102.
235
Riley E. P. Fetal alcohol spectrum disorders: an overview // Neuropsychology Review. 2013. Vol. 21. No. 2. Pp. 73–80.
236
Kesmodel U. S. The effect of different alcohol drinking patterns in early to mid pregnancy on the child’s intelligence, attention, and executive function // BJOG. 2012. Vol. 119. No. 10. Pp. 1180–1190.
237
Popova S. Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: a systematic review and meta-analysis // The Lancet. 2017. Vol. 5. Pp. e290–e299.
238
Goldstein R. F. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis // JAMA. 2017. Vol. 317. No. 21. Pp. 2207–2225.
239
По российским рекомендациям дополнительная потребность в энергии у беременных составляет 350 ккал в день во второй половине беременности. Прим. науч. ред.
241
Tam C. H. The impact of maternal gestational weight gain on cardiometabolic risk factors in children // Diabetologia. 2018. Vol. 61. No. 12. Pp. 2539–2548.
242
Allen-Walker V. Routine weighing of women during pregnancy — is it time to change current practice? // BJOG. 2015. Vol. 123. No. 6. Pp. 871–874.
243
Hytten F. Is it important or even useful to measure weight gain in pregnancy? // Midwifery. 1990. Vol. 6. No. 1. Pp. 28–32; Dawes M. G. Repeated measurement of maternal weight during pregnancy. Is this a useful practice? // BJOG. 1991. Vol. 98. No. 2. Pp. 189–194.
244
nhs.uk/common-health-questions/pregnancy/how-much-weight-will-i-put-on-during-my-pregnancy/ (18 October 2018).
245
Dalrymple K. V. Lifestyle interventions in overweight and obese pregnant or postpartum women for weight management: a systematic review // Nutrients. 2018. Vol. 10. No. 11. P. e1704.
246
Alvarado-Esquivel C. Miscarriage history and Toxoplasma gondii infection: a cross-sectional study in women in Durango City, Mexico // European Journal of Microbiology and Immunology. 2014. Vol. 4. No. 2. Pp. 117–122; Roberts F. Histopathological features of ocular toxoplasmosis in the fetus and infant // Archives of Ophthalmology. 2001. Vol. 119. No. 1. Pp. 51–58.
247
nhs.uk/conditions/pregnancy-and-baby/foods-to-avoid-pregnant/ (23 January 2017).
248
Действительно, в России нет рекомендаций об исключении копченых продуктов из рациона беременных. Прим. науч. ред.
249
Villazanakretzer D. L. Fish parasites: a growing concern during pregnancy // Obstetrical & Gynecological Survey. 2016. Vol. 71. No. 4. Pp. 253–259.
250
Taylor C. M. A review of guidance on fish consumption in pregnancy: is it fit for purpose? // Public Health Nutrition. 2018. Vol. 21. No. 11. Pp. 2149–2159.
251
Solan T. D. Mercury exposure in pregnancy: a review // Journal of Perinatal Medicine. 2014. Vol. 42. No. 6. Pp. 725–729.
252
Ebel E. Estimating the annual fraction of eggs contaminated with Salmonella enteritidis in the United States // International Journal of Food Microbiology. 2000. Vol. 61. No. 1. Pp. 51–62.
253
Gyang A. Salmonella Mississippi: a rare cause of second trimester miscarriage // Archives of Gynecology and Obstetrics. 2008. Vol. 277. No. 5. Pp. 437–438; Ravneet K. A case of Salmonella typhi infection leading to miscarriage // Journal of Laboratory Physicians. 2011. Vol. 3. No. 1. Pp. 61–62; Majowicz S. E. The global burden of nontyphoidal salmonella gastroenteritis // Clinical Infectious Diseases. 2010. Vol. 50. No. 6. Pp. 882–889.
254
bbc.co.uk/news/magazine-32033409 (25 March 2015).
255
Awofisayo A. Pregnancy-associated listeriosis in England and Wales // Epidemiology and Infection. 2015. Vol. 143. No. 2. Pp. 249–256.
256
Знак «Красный лев» ставится на яйцах, которые производятся по особому стандарту, позволяющему максимально снизить риск заражения сальмонеллезом, эти яйца разрешено есть сырыми даже уязвимым категориям граждан (к которым относятся дети и беременные). В частности, стандарт подразумевает обязательную вакцинацию кур от сальмонеллеза. Прим. науч. ред.
257
Madjunkov M. Listeriosis during pregnancy // Archives of Gynecology and Obstetrics. 2017. Vol. 296. No. 2. Pp. 143–152.
258
cdc.gov/listeria/technical.html (12 December 2016).
259
Fox M. Prepared salads recalled for salmonella, listeria risk // NBC News. 19 October 2018.
260
Withers M. Traditional beliefs and practices in pregnancy, childbirth and postpartum: a review of the evidence from Asian countries // Midwifery. 2018. Vol. 56. Pp. 158–170.
261
Nagata C. Hot — cold foods in diet and all-cause mortality in a Japanese community: the Takayama study // Annals of Epidemiology. 2017. Vol. 27. No. 3. Pp. 194–199.
262
Koren O. Host remodeling of the gut microbiome and metabolic changes during pregnancy // Cell. 2012. Vol. 150. No. 3. Pp. 470–480; Thornburn A. N. Evidence that asthma is a developmental origin disease influenced by maternal diet and bacterial metabolites // Nature Communications. 2015. Vol. 6. P. 7320.
263
cdc.gov/healthcommunication/toolstemplates/entertainmented/tips/Allergies.html (12 August 2019).
264
Gupta R. S. Prevalence and severity of food allergies among US adults // JAMA Netw. Open. 2019. Vol. 2. No. 1. P. e185630.
265
Love S. Food intolerance tests are shoddy science and traps for disordered eating // Vice. 23 February 2018.
266
Wenyin L. The epidemiology of food allergy in the global context // International Journal of Environmental Research and Public Health. 2018. Vol. 15. No. 9. P. 2043.
267
Hammond C. Unproven diagnostic tests for food allergy // Immunology and Allergy Clinics of North America. 2018. Vol. 31. No. 1. Pp. 153–163.
268
Venkataram D. Prevalence and longitudinal trends of food allergy during childhood and adolescence: results of the Isle of Wight Birth Cohort study // Clinical and Experimental Allergy. 2018. Vol. 48. No. 4. Pp. 394–402.
269
Yousef E. Clinical utility of serum specific IgE food testing in general practice: a tertiary care experience // Journal of Allergy and Clinical Immunology. 2019. Vol. 143. No. 2. P. AB275.
270
Описанный метод — это аллерген-специфическая иммунотерапия (АСИТ-терапия). Основы этой методики разработаны в 1911 году врачами Леонардом Нуном и Джоном Фриманом. Прим. науч. ред.
271
Vickery B. P. AR101 oral immunotherapy for peanut allergy // New England Journal of Medicine. 2018. Vol. 379. No. 21. Pp. 1991–2001.
272
Pretorius R. A. Maternal fiber dietary intakes during pregnancy and infant allergic disease // Nutrients. 2019. Vol. 11. No. 8. P. 1767.
273
Eigenmann P. A. Are avoidance diets still warranted in children with atopic dermatitis? // Pediatric Allergy and Immunology. 2020. Vol. 1. Pp. 19–26.
274
Овес содержит белок из группы проламинов авенин, его структура отличается от структуры глютена пшеницы. Для большинства больных целиакией употребление овса не опасно. Прим. науч. ред.
275
Lebwohl B. Long term gluten consumption in adults without celiac disease and risk of coronary heart disease: prospective cohort study // BMJ. 2017. Vol. 357. P. j1892.
276
Volta U. High prevalence of celiac disease in Italian general population // Digestive Diseases and Science. 2011. Vol. 46. No. 7. Pp. 1500–1505.
277
Biesiekierski J. R. Non-coeliac gluten sensitivity: piecing the puzzle together // United European Gastroenterology. 2015. Vol. 3. No. 2. Pp. 160–165.
278
Melini V. Gluten-free diet: gaps and needs for a healthier diet // Nutrients. 2019. Vol. 11. No. 1. P. 170.
279
Johnston C. S. Commercially available gluten-free pastas elevate postprandial glycemia in comparison to conventional wheat pasta in healthy adults: a double-blind randomized crossover trial // Food Funct. 2017. Vol. 8. No. 9. Pp. 3139–3144.
280
Croall I. D. Gluten does not induce gastrointestinal symptoms in healthy volunteers: a double-blind randomized placebo trial // Gastroenterology. 2019. Vol. 157. Pp. 881–883.
281
Roager H. M. Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: a randomised cross-over trial // Gut. 2019. Vol. 68. Pp. 83–93.
282
UK exercise guidelines: nhs.uk/live-well/exercise/ (30 May 2018); US exercise guidelines: health.gov/paguidelines/ (2019)
283
Tigbe W. W. Time spent in sedentary posture is associated with waist circumference and cardiovascular risk // International Journal of Obesity. 2017. Vol. 41. No. 5. Pp. 689–696.
284
Fujita H. Physical activity earlier in life is inversely associated with insulin resistance among adults in Japan // Journal of Epidemiology. 2019. Vol. 29. No. 2. Pp. 57–60.
285
Pontzer H. Hunter-gatherer energetics and human obesity // PLOS ONE. 2012. Vol. 7. No. 7. P. e40503.
286
Casanova N. Metabolic adaptations during negative energy balance and potential impact on appetite and food intake // Proceedings of the Nutrition Society. 2019. Vol. 78. No. 3. Pp. 279–289.
287
Thomas D. M. Why do individuals not lose more weight from an exercise intervention at a defined dose? An energy balance analysis // Obesity Reviews. 2013. Vol. 13. No. 10. Pp. 835–847.
288
Mostrous A. Coca-Cola spends £10m to counter links with obesity // The Times. 18 December 2015; Gornall J. Sugar: spinning a web of influence // BMJ. 2015. Vol. 350. P. h231.
289
Nestle M. Unsavory Truth: How Food Companies Skew the Science of What We Eat. Basic Books, 2018.
290
Noakes T. D. Lobbyists for the sports drink industry: example of the rise of “contrarianism” in modern scientific debate // Br. J. of Sports Med. 2007. Vol. 41. No. 2. Pp. 107–109.
291
Burke L. M. Swifter, higher, stronger: What’s on the menu? // Science. 2018. Vol. 362. No. 6416. Pp. 781–787.
292
Chekroud S. R. Association between physical exercise and mental health in 1.2 million individuals in the USA between 2011 and 2015 // Lancet Psychiatry. 2018. Vol. 5. Pp. 739–746.
293
Gustafson C. R. Exercise and the timing of snack choice: healthy snack choice is reduced in the post-exercise state // Nutrients. 2018. Vol. 10. No. 12. P. 1941.
294
Флуоксетин (прозак) — популярный антидепрессант, селективный ингибитор обратного захвата серотонина. Прим. науч. ред.
295
Jakubovski E. Systematic review and meta-analysis: dose-response relationship of selective-serotonin reuptake inhibitors in major depressive disorder // American Journal of Psychiatry. 2016. Vol. 173. No. 2. Pp. 174–183.
296
Lai J. S. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults // American Journal of Clinical Nutrition. 2014. Vol. 99. No. 1. Pp. 181–197; Recchia D. Associations between long-term adherence to healthy diet and recurrent depressive symptoms in Whitehall II Study // European Journal of Nutrition. 2019. Vol. 1. Pp. 1–11.
297
Reynolds C. F. Early intervention to preempt major depression in older black and white adults // Psychiatric Services. 2014. Vol. 65. No. 6. Pp. 765–773.
298
Jacka F. N. A randomised controlled trial of dietary improvement for adults with major depression (the “SMILES” trial) // BMC Medicine. 2017. Vol. 15. No. 1. P. 23.
299
Firth J. The effects of dietary improvement on symptoms of depression and anxiety: a meta-analysis of randomized controlled trials // Psychosomatic Medicine. 2019. Vol. 81. No. 3. Pp. 265–280; Mizuno S. Bifidobacterium-rich fecal donor may be a positive predictor for successful fecal microbiota transplantation in patients with irritable bowel syndrome // Digestion. 2017. Vol. 96. No. 1. Pp. 29–38.
300
Sánchez-Villegas A. Mediterranean dietary pattern and depression: the PREDIMED randomized trial // BMC Medicine. 2013. Vol. 11. P. 208.
301
Valles Colomer M. The neuroactive potential of human gut microbiota in quality of life and depression // Nature Microbiology. 2019. Vol. 4. Pp. 623–632.
302
Yano J. M. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis // Cell. 2015. Vol. 161. No. 2. Pp. 264–276.
303
Lukić I. Antidepressants affect gut microbiota and Ruminococcus flavefaciens is able to abolish their effects on depressive-like behavior // Translational Psychiatry. 2019. Vol. 9. No. 1. P. 133.
304
Walters M. J. Associations of lifestyle and vascular risk factors with Alzheimer’s brain biomarkers during middle age // BMJ OPEN. 2018. Vol. 8. No. 11. P. e023664.
305
Akbaraly T. Association of long-term diet quality with hippocampal volume: longitudinal cohort study // American Journal of Medicine. 2018. Vol. 131. No. 11. Pp. 1372–1381.
306
Setti S. E. Alterations in hippocampal activity and Alzheimer’s disease // Translational Issues in Psychological Science. 2018. Vol. 3. No. 4. Pp. 348–356.
307
Глутаминовая кислота (глутомат) — возбуждающий нейромедиатор. ГАМК — гамма-аминомасляная кислота — тормозной нейромедиатор нервной системы млекопитающих. Прим. науч. ред.
308
Zheng P. The gut microbiome from patients with schizophrenia modulates the glutamate-glutamine-GABA cycle and schizophrenia-relevant behaviors in mice // Science Advances. 2019. Vol. 5. No. 2. P. eaau8317.
309
Argou-Cardozo I. Clostridium bacteria and autism spectrum conditions: a systematic review and hypothetical contribution of environmental glyphosate Levels // Medical Sciences. 2018. Vol. 6. No. 2. P. 29.
310
Kang D. W. Differences in fecal microbial metabolites and microbiota of children with autism spectrum disorders // Anaerobe. 2018. Vol. 49. Pp. 121–131.
311
Mizuno S. Bifidobacterium-rich fecal donor may be a positive predictor for successful fecal microbiota transplantation in patients with irritable bowel syndrome // Digestion. 2017. Vol. 96. No. 1. Pp. 29–38.
312
Butler M. I. From isoniazid to psychobiotics: the gut microbiome as a new antidepressant target // British Journal of Hospital Medicine. 2019. Vol. 80. No. 3. Pp. 139–145.
313
Jacka F. N. Maternal and early postnatal nutrition and mental health of offspring by age 5 years: a prospective cohort study // J. Acad. Child & Adol. Psych. 2013. Vol. 52. No. 10. Pp. 1038–1047.
314
Jacka F. Brain Changer: How diet can save your mental health. Yellow Kite, 2019.
315
Saylor A. What’s wrong with the tap? Examining perceptions of tap water and bottled water at Purdue University // Environmental Management. 2011. Vol. 48. No. 3. Pp. 588–601.
316
Lantagne D. Household water treatment and cholera control // Journal of Infectious Diseases. 2018. Vol. 218. No. 3. Pp. s147–s153.
317
McCartney M. Waterlogged? // BMJ. 2011. Vol. 343. P. d4280.
318
Rosario-Ortiz F. How do you like your tap water? // Science. 2016. Vol. 351. No. 6267. Pp. 912–914.
319
Brezina E. Investigation and risk evaluation of the occurrence of carbamazepine, oxcarbazepine, their human metabolites and transformation products in the urban water cycle // Environmental Pollution. 2017. Vol. 225. Pp. 261–269.
320
Spector T. Identically Different. Weidenfeld & Nicolson, 2012.
321
Wagner M. Identification of putative steroid receptor antagonists in bottled water // PLOS ONE. 2013. Vol. 8. No. 8. P. e72472.
322
Huo W. Maternal urinary bisphenol A levels and infant low birth weight: a nested case-control study of the Health Baby Cohort in China // Environmental International. 2015. Vol. 85. Pp. 96–103; Gao H. Bisphenol A and hormone-associated cancers: current progress and perspectives // Medicine. 2015. Vol. 94. No. 1. P. e211.
323
EFSA. Bisphenol A: new immune system evidence useful but limited // EFSA Reports. 13 October 2016.
324
Iheozor-Ejiofor Z. Water fluoridation for the prevention of dental caries // Cochrane Database of System Reviews. 2015. Vol. 6. P. CD010856.
325
Jambeck J. R. Marine pollution. Plastic waste inputs from land into the ocean // Science. 2015. 13. Vol. 347. No. 6223. Pp. 768–771.
326
Ryan P. G. Monitoring the abundance of plastic debris in the marine environment // Proceedings Transactions Royal Soc. B. 2009. Vol. 364. Pp. 1999–2012.
327
Bartoshuk L. M. NaCl thresholds in man: thresholds for water taste or NaCl taste? // Journal of Comparative and Physiological Psychology. 1974. Vol. 87. No. 2. Pp. 310–325.
329
Lachenmeier D. W. Comparative risk assessment of alcohol, tobacco, cannabis and other illicit drugs using the margin of exposure approach // Scientific Reports. 2015. Vol. 5. P. 8126.
330
Bruha R. Alcoholic liver disease // World Journal of Hepatology. 2012. Vol. 4. No. 3. Pp. 81–90; Jordaan G. P. Alcohol-induced psychotic disorder: a review // Metabolic Brain Disease. 2014. Vol. 29. No. 2. Pp. 231–243.
332
St Leger A. S. Factors associated with cardiac mortality in developed countries with particular reference to the consumption of wine // Lancet. 1979. Vol. 1. No. 8124. Pp. 1017–1020; Di Castelnuovo A. Alcohol dosing and total mortality in men and women: an updated meta-analysis // Archives of Internal Medicine. 2006. Vol. 166. No. 22. Pp. 2437–2445.
333
gov.uk/government/news/new-alcohol-guidelines-show-increased-risk-of-cancer (8 January 2016).
334
Xi B. Relationship of alcohol consumption to all-cause, cardiovascular, and cancerrelated mortality in US adults // J. American College of Cardiology. 2017. Vol. 70. No. 8. Pp. 913–922.
335
Welch K. A. Alcohol consumption and brain health // BMJ. 2017. Vol. 357. P. j2645.
336
Sabia S. Alcohol consumption and risk of dementia: 23 year follow-up of Whitehall II cohort study // BMJ. 2018. Vol. 362. P. k2927.
337
Holt-Lunstad J. Social relationships and mortality risk: a meta-analytic review // PLOS Medicine. 2010. Vol. 7. No. 7. P. e1000316.
338
Wood A. M. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599,912 current drinkers in 83 prospective studies // The Lancet. 2018. Vol. 391. No. 10129. Pp. 1513–1523.
339
Griswold M. G. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016 // The Lancet. 2018. Vol. 392. No. 10152. Pp. 1015–1035.
340
Freeman A. L. Communicating health risks in science publications: time for everyone to take responsibility // BMC Medicine. 2018. Vol. 16. No. 1. P. 207.
341
Edenberg H. J. The genetics of alcohol metabolism: role of alcohol dehydrogenase and aldehyde dehydrogenase variants // Alcohol Research and Health. 2007. Vol. 30. No. 1. Pp. 5–13.
342
Ruiz S. M. Closing the gender gap: the case for gender-specific alcoholism research // Journal of Alcoholism and Drug Dependence. 2013. Vol. 1. No. 6. P. e106.
343
Vatsalya V. A review on the sex differences in organ and system pathology with alcohol drinking // Current Drug Abuse Reviews. 2017. Vol. 9. No. 2. Pp. 87–92.
344
Lloyd P. Deadly link between alcohol and breast cancer is “ignored by middleaged women who are most at risk of developing the disease” // Mail Online. 13 February 2019.
345
Queipo-Ortuño M. I. Influence of red wine polyphenols and ethanol on the gut microbiota ecology and biomarkers // Am. Journal of Clinical Nutrition. 2012. Vol. 95. No. 6. Pp. 1323–1334.
346
Chaplin A. Resveratrol, metabolic syndrome, and gut microbiota // Nutrients. 2018. Vol. 10. No. 11. P. e1651; Fan X. Drinking alcohol is associated with variation in the human oral microbiome in a large study of American adults // Microbiome. 2018. Vol. 6. No. 1. P. 59.
347
LeRoy C. I. Red wine consumption associated with increased gut microbiota α-diversity in 3 independent cohorts // Gastroenterology. 2019. Vol. pii: S0016–5085. No. 19. Pp. 41244–4.
348
de Visser R. O. The growth of “Dry January”: promoting participation and the benefits of participation // Eur. J. Public Health. 2017. Vol. 27. No. 5. Pp. 929–931.
349
Naimi T. S. Erosion of state alcohol excise taxes in the United States // Journal of Studies on Alcohol and Drugs. 2018. Vol. 79. No. 1. Pp. 43–48.
350
cdc.gov/alcohol/index.htm (2019).
351
Zupan Z. Erosion of state alcohol excise taxes in the United States // BMJ. 2017. Vol. 359. P. j5623.
352
Coley D. Local food, food miles and carbon emissions: a comparison of farm shop and mass distribution approaches // Food Policy. 2009. Vol. 34. No. 2. Pp. 150–155.
353
Saunders C. Food miles, carbon footprinting and their potential impact on trade // Semantic Scholar. 2009; AARES 53rd annual conference at Cairns, 10–13 February 2009.
354
Soode-Schimonsky E. Product environmental footprint of strawberries: case studies in Estonia and Germany // J. Environ. Management. 2017. Vol. 203. Pt. 1. Pp. 564–577.
355
Willett W. Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems // The Lancet. 2019. Vol. 393. No. 10170. Pp. 447–492.
356
Milner J. Health effects of adopting low greenhouse gas emission diets in the UK // BMJ Open. 2015. Vol. 5. P. e007364.
357
Poore J. Reducing food’s environmental impacts through producers and consumers // Science. 2018. Vol. 360. Pp. 987–992.
358
Searchinger T. D. Assessing the efficiency of changes in land use for mitigating climate change // Nature. 2018. Vol. 564. Pp. 249–253.
359
Monbiot G. We can’t keep eating as we are — why isn’t the IPCC shouting this from the rooftops? // The Guardian. 9 August 2019.
360
Mesnage R. Facts and fallacies in the debate on glyphosate toxicity // Frontiers in Public Health. 2017. Vol. 5. P. 316.
361
iarc.fr/wp-content/uploads/2018/07/MonographVolume112–1.pdf (20 March 2015).
362
Webster B. Weedkiller scientist was paid £120,000 by cancer lawyers // The Times. 18 October 2017.
363
Mills P. J. Excretion of the herbicide glyphosate in older adults between 1993 and 2016 // JAMA. 2017. Vol. 318. No. 16. Pp. 1610–1611.
364
Tarazona J. V. Glyphosate toxicity and carcinogenicity: a review of the scientific basis of the European Union assessment and its differences with IARC // Archives of Toxicology. 2017. Vol. 91. No. 8. Pp. 2723–2743; Portier C. J. Update to Tarazona et al. (2017): glyphosate toxicity and carcinogenicity: a review of the scientific basis of the European Union assessment and its differences with IARC // Archives of Toxicology. 2018. Vol. 92. No. 3. P. 1341.
365
Chang E. T. Systematic review and meta-analysis of glyphosate exposure and risk of lymphohematopoietic cancers // Journal of Environmental Science and Health, Part B. 2016. Vol. 51. No. 6. Pp. 402–434.
366
Gillezeau C. The evidence of human exposure to glyphosate: a review // Environmental Health. 2019. Vol. 18. No. 1. P. 2; Leon M. E. Pesticide use and risk of non-Hodgkin lymphoid malignancies in agricultural cohorts from France, Norway and the USA: a pooled analysis from the AGRICOH consortium // International Journal of Epidemiology. 2019. Vol. 48. No. 5. Pp. 1519–1535.
367
Hu L. The association between non-Hodgkin lymphoma and organophosphate pesticides exposure: a meta-analysis // Environmental Pollution. 2017. Vol. 231. Pp. 319–328.
368
González-Alzaga B. A systematic review of neurodevelopmental effects of prenatal and postnatal organophosphate pesticide exposure // Toxicology Letters. 2014. Vol. 230. No. 2. Pp. 104–121; Chiu Y. Association between pesticide residue intake from consumption of fruits and vegetables and pregnancy outcomes among women undergoing infertility treatment with assisted reproductive technology // JAMA. 2018. Vol. 178. No. 1. Pp. 17–26.
369
Manservisi F. The Ramazzini Institute 13-week pilot study glyphosate-based herbicides administered at human-equivalent dose to Sprague Dawley rats // Environmental Health. 2019. Vol. 18. No. 1. P. 15; Aitbali Y. Glyphosate-based herbicide exposure affects gut microbiota, anxiety and depression-like behaviors in mice // Neurotoxicology and Teratology. 2018. Vol. 67. Pp. 44–49.
370
Motta E. V. Glyphosate perturbs the gut microbiota of honey bees // PNAS. 2018. Vol. 115. No. 41. Pp. 10305–10310.
371
Baudry J. Association of frequency of organic food consumption with cancer risk: findings from NutriNet-Santé Prospective Cohort Study // JAMA. 2018. Vol. 178. No. 12. Pp. 1597–1606.
372
Bradbury K. E. Organic food consumption and the incidence of cancer in a large prospective study of women in the UK // British Journal of Cancer. 2014. Vol. 110. Pp. 2321–2326.
373
anh-usa.org/wp-content/uploads/2016/04/ANHUSA-glyphosate-breakfast-study-FINAL.pdf (19 April 2016)
374
Womersley K. Medical schools should be prioritising nutrition and lifestyle education // BMJ. 2017. Vol. 359. P. j4861.
375
Crowley J. Nutrition in medical education: a systematic review // Lancet Planetary Health. 2019. Vol. 9. P. PE379–E389.
376
Greenhalgh S. Making China safe for Coke: how Coca-Cola shaped obesity science and policy in China // BMJ. 2019. Vol. 364. P. k5050.
377
Lean M. E. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial // The Lancet. 2018. Vol. 391. No. 10120. Pp. 541–551.
378
ncbi.nlm.nih.gov/pubmed/21366836; Zhu D. The relationship between health professionals’ weight status and attitudes towards weight management: a systematic review // Obesity Reviews. 2011. Vol. 12. No. 5. Pp. e324–337.
380
Aspry K. E. Medical nutrition education, training and competencies to advance guideline-based diet counseling by physicians // Circulation. 2018. Vol. 137. Pp. e821–e841.
381
McDonald D. American gut: an open platform for citizen science microbiome research // mSystems. 2018. Vol. 3. No. 3. Pp. e00031–18.
382
383
Blaser M. J. Antibiotic use and its consequences for the normal microbiome // Science. 2016. Vol. 352. Pp. 544–545.
384
de Cabo R. Effects of intermittent fasting on health, aging and disease // New England Journal of Medicine. 2019. Vol. 381. Pp. 2541–2551.
385
US Burden of Disease Collaborators. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors // JAMA. 2013. Vol. 310. No. 6. Pp. 591–606.
386
Reiley L. How the Trump administration limited the scope of the USDA’s 2020 dietary guidelines // Washington Post. 30 August 2019.
387
Sterk R. EU Sugar producers suffer after reform // Food Business News. 8 August 2019.
388
Moses H. The anatomy of medical research: US and international comparisons // JAMA. 2015. Vol. 313. No. 2. Pp. 174–189.
389
Kyle R. G. Obesity prevalence among healthcare professionals in England: a cross sectional study using the Health Survey for England // BMJ Open. 2017. 4 Dec. P. 018498; Luckhaupt S. E. Prevalence of obesity among US workers and associations with occupational factors // Am. J. Prev. Med. 2014. Vol. 46. No. 3. Pp. 237–248.

Чихание, больное горло, насморк – все знают первые неприятные признаки простуды. Почему мы так легко простужаемся? Какие грозные заболевания умеют маскироваться под обычную простуду? Можно ли и как предупредить и вылечить простуду без лекарств? Когда помогут домашние средства, а когда надо немедленно обращаться к врачу? Как уберечь от простуды детей? На эти и многие другие вопросы вы найдете ответы в этой книге. Вы узнаете об иммунной системе человека и естественных способах ее тренировки: закаливании, физических упражнениях, воздействии факторов природы, правильном питании.

В книге рассказывается история главного героя, который сталкивается с различными проблемами и препятствиями на протяжении всего своего путешествия. По пути он встречает множество второстепенных персонажей, которые играют важные роли в истории. Благодаря опыту главного героя книга исследует такие темы, как любовь, потеря, надежда и стойкость. По мере того, как главный герой преодолевает свои трудности, он усваивает ценные уроки жизни и растет как личность.
В рейтинге самых здоровых людей в Европе шведы занимают первое место. В чем же их секрет? Только ли в том, что они любят движение, предпочитают полезную пищу и занимаются своим здоровьем с детства? Шведский врач Бертил Марклунд попытался разобраться в том, что же делает шведов такими здоровыми. Вопреки расхожему мнению, он считает, что на здоровье влияет не столько наследственность, сколько образ жизни. Выходит, что мы можем сами управлять своим самочувствием, сами решать, сколько лет прожить, как стареть и стареть ли вообще. В этой книге доктор Бертил Марклунд сосредоточился не на болезнях, а на мерах поддержания здоровья.

Фастфуд – это не только гамбургер и пачка чипсов. Это практически любая еда, выпущенная промышленным способом. Эрик Шлоссер стирает грань между заведениями быстрого питания и прилавками магазинов, где мы покупаем еду. С впечатляющей дотошностью он изобличает индустриальные технологии производства продуктов питания, вскрывая все шокирующие, противоестественные и антигуманные подробности того, как в современном мире производится еда. Эта невероятная книга поможет вам заглянуть за кулисы пищевой индустрии, понять, что именно вы едите, и начать принимать более осознанные решения при выборе продуктов питания для себя и своей семьи. На русском языке публикуется впервые.

Большой количество писем, подтолкнули меня к созданию этого тома. Не знаю, решусь ли я еще продолжить эту тему… Но то, что получилось — все вам, мои читатели. Пусть это будет и советами, и чтением на каждый день.
Курение – это привычка, и в то же время навязчивая химическая и эмоциональная зависимость, которую вы тесно увязываете с вашей повседневной деятельностью и сценариями жизни. Когда-то вы придали курению эмоциональную привлекательность, приписали его к зоне комфорта, сделали тем, что вам нравится. Таким образом, вы полностью заблокировали критическое отношение к курению. Очевидное проявление разрушительных последствий курения растянуто во времени и может быть значительно отстроченным, это также затрудняет адекватную оценку вреда этой привычки самим курильщиком.
Что такое настоящая, здоровая еда? Это вовсе не те продукты, что мы видим в магазинах, – в привлекательных упаковках и заявленные как полезные для здоровья. Майкл Поллан призывает перестать изучать списки труднопроизносимых ингредиентов на упаковках, отказаться от модных диет и заново разобраться, что же такое правильное питание. Следуя его простым советам, вы сможете составить оптимальный именно для вас рацион, чтобы поддерживать хорошее самочувствие и быть счастливыми. На русском языке публикуется впервые.
В этой книге акушер-гинеколог Дженнифер Линкольн делится своим опытом: развенчивает распространенные мифы о женском интимном здоровье, рассказывает о работе гормонов, гигиене, противозачаточных средствах и многом другом. Читательницы найдут ответы на волнующие их вопросы и смогут сделать важный выбор — в пользу здоровья и искренней заботы о себе. Книга подготовлена в информационных целях. Перед применением приведенных рекомендаций обязательно проконсультируйтесь с врачом.
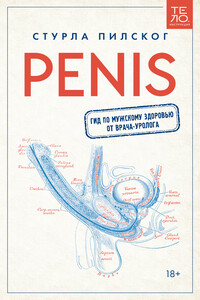
В легкой и увлекательной форме норвежский уролог Стурла Пилског рассказывает о том, как устроена мочеполовая система у мужчин. Эта книга ответит на самые волнующие вопросы, научит отличать опасные состояния от нормальных и объяснит, что можно сделать, чтобы избавиться от проблем. На русском языке публикуется впервые.
Правильно питаться, больше двигаться, уменьшить стресс и сильнее любить – эти несложные правила не только сделают жизнь гармоничной, но и помогут предотвратить развитие целого ряда заболеваний. Однако соблюдать их бывает очень непросто. Дин Орниш, диетолог семьи Клинтон, вместе с супругой Энн просто и понятно рассказывают о том, почему эти правила работают, как внедрить их в свою жизнь, какие препятствия поджидают на этом пути и как с ними бороться. Для всех, кто заботится о своем здоровье и мечтает прожить долгую и счастливую жизнь. На русском языке публикуется впервые.